Key Takeaways
- While tinnitus itself doesn’t directly cause dizziness, both symptoms often occur together due to underlying inner ear disorders.
- Conditions like Ménière’s disease, vestibular migraines, and acoustic neuromas commonly trigger both tinnitus and dizziness symptoms.
- The inner ear houses both hearing and balance mechanisms, explaining why problems can affect both functions simultaneously.
- Research shows up to 30% of people with tinnitus also experience some form of dizziness or vertigo.
- MindEar offers comprehensive solutions for those suffering from tinnitus-related symptoms that can impact quality of life.
That ringing in your ears suddenly has company—the room is spinning. Is it just a coincidence, or could your tinnitus actually be causing your dizziness? This question brings countless people to search for answers as they navigate these disruptive symptoms.
If you’re experiencing both tinnitus and dizziness, you’re not alone. According to research from MindEar, these symptoms frequently appear together, though their relationship is more complex than simple cause and effect. Understanding this connection could be the key to finding relief.
When Ringing in Your Ears Makes the Room Spin: Tinnitus and Dizziness
“Ringing in Ears, Dizziness, Pressure …” from www.healthline.com and used with no modifications.
Tinnitus—that persistent ringing, buzzing, or hissing sound in your ears—affects millions of people worldwide. Similarly, dizziness is one of the most common reasons adults visit their doctors. When both symptoms occur simultaneously, it can significantly impact daily life, making simple tasks feel overwhelming and even dangerous.
While tinnitus doesn’t directly cause dizziness, they often share common origins, particularly in the delicate structures of your inner ear. This connection explains why treating one symptom may sometimes help relieve the other.
The relationship between these symptoms isn’t always straightforward. Sometimes they appear together immediately, while in other cases, one symptom might precede the other by weeks or months. This variation depends largely on the underlying condition affecting your ear or neurological system.
The Science Behind Tinnitus-Related Dizziness
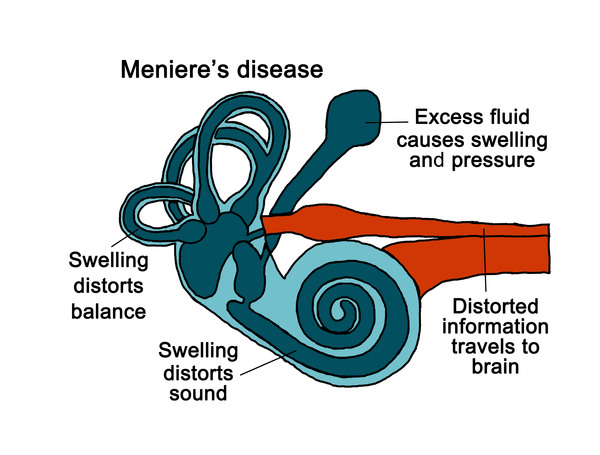
“Ménière disease: MedlinePlus Genetics” from medlineplus.gov and used with no modifications.
To understand why tinnitus and dizziness frequently coexist, we need to explore the remarkable design of our ears. These complex organs do far more than just help us hear—they’re also essential for maintaining our balance and spatial orientation.
How Your Ear Controls Both Hearing and Balance
Your inner ear houses two critical systems that work in remarkable harmony. The cochlea transforms sound waves into electrical signals for your brain to interpret as sound. Just adjacent to this hearing center sits the vestibular system—three semicircular canals and two otolith organs filled with fluid and tiny hair cells that detect head movements and position.
These systems share more than just proximity—they share blood supply, fluid dynamics, and neural connections. When something disrupts the inner ear environment, both systems can be affected simultaneously. This explains why conditions affecting the inner ear often produce both auditory symptoms (like tinnitus) and balance issues (like dizziness or vertigo).
The relationship is further complicated by the brain’s processing centers. Your brain integrates signals from your ears, eyes, and body position sensors to maintain balance. When tinnitus occurs, it can sometimes interfere with this integration, potentially contributing to feelings of disorientation or unsteadiness.
Why Tinnitus and Dizziness Often Occur Together
Several factors explain the frequent co-occurrence of these symptoms. First, damage to the inner ear hair cells—whether from noise exposure, aging, or other causes—can affect both hearing and balance functions. Second, conditions that alter fluid pressure in the inner ear, like Ménière’s disease, typically produce both tinnitus and vertigo as primary symptoms.
The connection extends to the central nervous system as well. Your brain’s ability to compensate for inner ear dysfunction plays a crucial role in symptom manifestation. Some people with inner ear damage experience primarily tinnitus, while others develop more pronounced dizziness, depending on individual neurological adaptation.
Psychological factors also contribute significantly. The stress and anxiety that often accompany tinnitus can trigger or worsen dizziness in susceptible individuals. This creates a challenging cycle where each symptom potentially amplifies the other. For those seeking relief, exploring natural treatment for tinnitus may offer effective solutions.
Research Statistics on Tinnitus-Dizziness Connection
Scientific literature provides compelling evidence of the relationship between these symptoms. Studies indicate that approximately 30% of people with tinnitus also experience some form of dizziness or balance issues. Conversely, among patients presenting with dizziness as their primary complaint, up to 20% report concurrent tinnitus.
A particularly revealing study published in the International Tinnitus Journal found that patients with both symptoms typically experienced more severe functional impairment than those with either symptom alone. This suggests that when tinnitus and dizziness occur together, they may have synergistic negative effects on quality of life.
Research Highlight: A 2018 systematic review analyzing 25 studies found that vestibular disorders were present in approximately 65% of patients who reported both tinnitus and dizziness, highlighting the inner ear as the common denominator in most cases.
5 Medical Conditions That Link Tinnitus and Dizziness
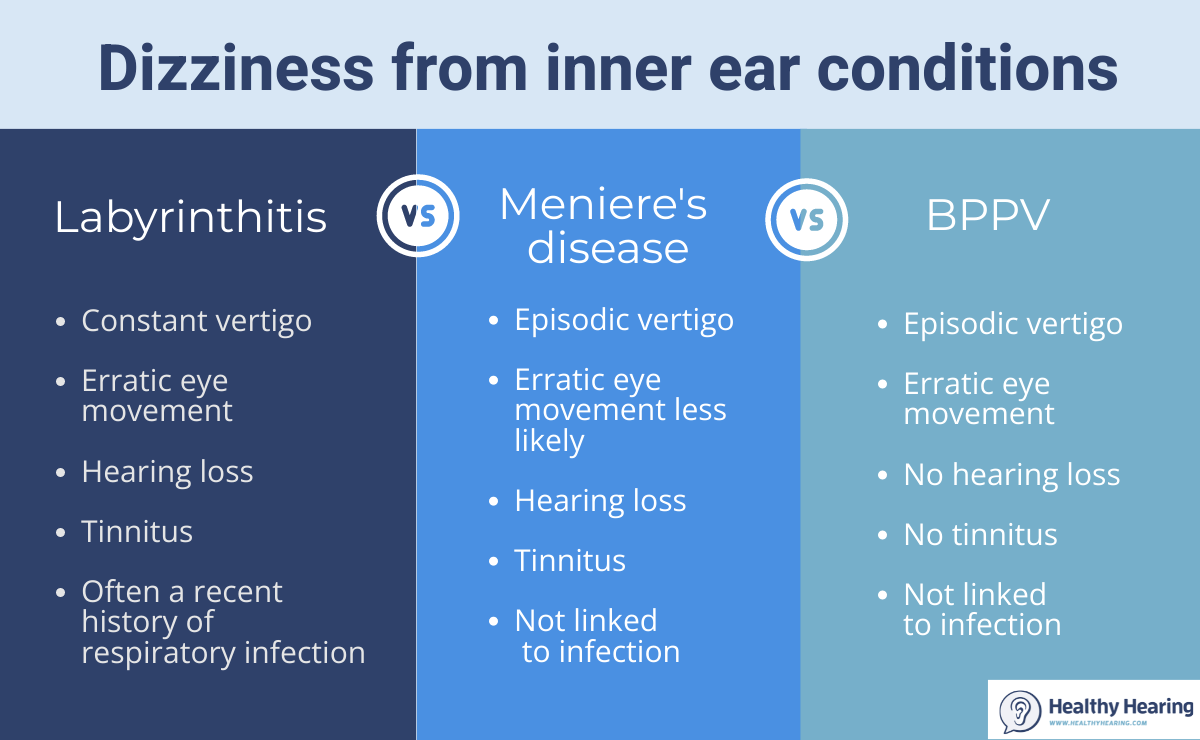
“Meniere’s, labyrinthitis, or BPPV? How …” from www.healthyhearing.com and used with no modifications.
Understanding specific conditions that cause both tinnitus and dizziness can help guide proper diagnosis and treatment. Each condition affects the ear differently, but all can disrupt both hearing and balance functions.
1. Ménière’s Disease: The Fluid Buildup Problem
Ménière’s disease stands as perhaps the most notorious condition linking tinnitus and dizziness. This inner ear disorder causes excessive fluid buildup (endolymph) in the labyrinth, creating pressure that affects both hearing and balance mechanisms. The classic symptoms include episodic vertigo attacks lasting from 20 minutes to several hours, fluctuating hearing loss, tinnitus, and a feeling of fullness in the affected ear.
2. Vestibular Migraines: When Headaches Affect Your Balance
Vestibular migraines represent a fascinating intersection between neurological and balance disorders. Unlike classic migraines, these specialized headaches prominently feature dizziness, vertigo, and balance disturbances as primary symptoms—sometimes even without headache pain. Approximately 40% of vestibular migraine patients also report tinnitus during episodes, making this condition a significant link between the two symptoms.
The mechanism behind vestibular migraines involves temporary changes in brain blood flow and neural activity that affect both auditory and vestibular processing centers. These episodes typically last hours to days and may be triggered by stress, certain foods, hormonal changes, or sleep disruption. Many patients describe a characteristic “rocking” or “floating” sensation accompanied by increased sensitivity to sound (including the perception of tinnitus) and motion sensitivity that can persist between acute attacks.
3. Acoustic Neuroma: Tumors That Disrupt Hearing and Balance
Acoustic neuromas (also called vestibular schwannomas) are benign tumors that develop on the vestibulocochlear nerve connecting the inner ear to the brain. As these slow-growing tumors expand, they compress both the auditory and balance portions of this nerve, creating a perfect storm for simultaneous tinnitus and dizziness. Early symptoms often begin with unilateral (one-sided) tinnitus and gradual hearing loss, followed by increasing unsteadiness and balance problems as the tumor enlarges. The distinctive pattern of progressive, one-sided symptoms makes acoustic neuromas an important consideration when tinnitus and dizziness occur together, particularly when hearing loss is also present on the affected side.
4. BPPV (Benign Paroxysmal Positional Vertigo)
BPPV represents one of the most common causes of vertigo, characterized by brief episodes of intense spinning sensations triggered by specific head movements. This condition occurs when calcium carbonate crystals (otoconia) become dislodged from their normal position and migrate into the semicircular canals of the inner ear. Though BPPV primarily causes positional dizziness, many patients report experiencing tinnitus either during vertigo episodes or as a separate chronic symptom.
The connection between BPPV and tinnitus likely stems from the shared inner ear environment and potential underlying damage to the vestibular system. Research suggests that approximately 20-30% of BPPV patients experience some degree of tinnitus, with higher prevalence among those with recurrent or severe cases. Interestingly, successful treatment of BPPV through repositioning maneuvers sometimes leads to improvement in tinnitus symptoms, highlighting the interconnected nature of these inner ear manifestations.
5. Superior Canal Dehiscence Syndrome
Superior Canal Dehiscence Syndrome (SCDS) results from an abnormal opening (dehiscence) in the bone covering the superior semicircular canal of the inner ear. This rare but increasingly recognized condition creates a “third window” effect that allows pressure and sound to affect the inner ear abnormally. Patients with SCDS often experience a distinctive constellation of symptoms including autophony (hearing one’s own voice, breathing, or even heartbeat abnormally loudly), dizziness triggered by loud sounds (Tullio phenomenon), and chronic tinnitus that may pulsate with heartbeat. The condition is particularly noteworthy because surgical repair of the bone defect can sometimes provide significant relief from both dizziness and tinnitus symptoms, demonstrating their shared mechanical origin in this disorder.
Medication Side Effects That Trigger Both Symptoms
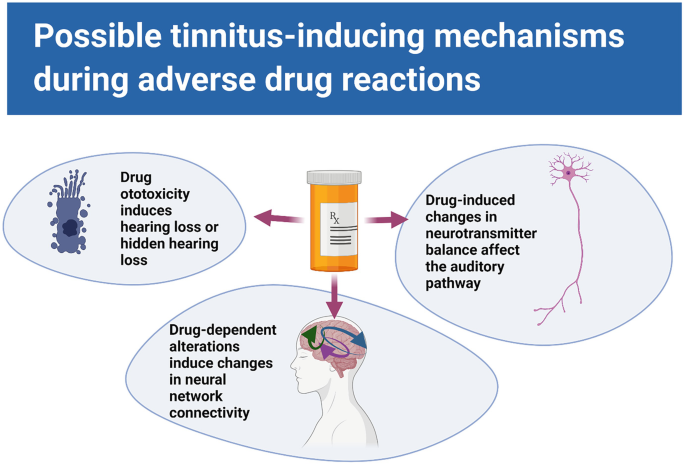
“Safety Pharmacology and Tinnitus …” from link.springer.com and used with no modifications.
Beyond anatomical and disease-related causes, numerous medications can induce both tinnitus and dizziness as unwanted side effects. These ototoxic (ear-damaging) medications typically affect the delicate hair cells within both the cochlea and vestibular apparatus, leading to dual symptoms that often develop gradually with continued use. In some cases, discontinuing the medication resolves both issues, while in others, the damage may be permanent. Understanding which medications carry these risks is crucial for both patients and healthcare providers, especially when alternative treatments might be available.
Common Drugs That Cause Tinnitus and Dizziness
Several medication classes stand out for their potential to cause both tinnitus and dizziness. High-dose aspirin and NSAIDs (non-steroidal anti-inflammatory drugs) can affect inner ear blood flow and fluid balance, while certain antibiotics—particularly aminoglycosides like gentamicin—directly damage sensory hair cells. Loop diuretics (furosemide, bumetanide) alter inner ear fluid composition, and chemotherapy agents, especially cisplatin and carboplatin, are notoriously ototoxic. Even common medications like certain antidepressants, antimalarials like quinine, and some antihypertensives can trigger or worsen both symptoms. The risk typically increases with higher doses, longer duration of use, and in patients with existing ear or kidney problems that affect drug clearance. For those looking for alternative approaches, exploring natural treatments for tinnitus may provide relief.
How to Tell if Your Medication is the Culprit
Identifying medication-induced tinnitus and dizziness involves careful attention to timing and patterns. Symptoms that begin shortly after starting a new medication or increasing dosage suggest a causal relationship, particularly if they improve when doses are reduced or medication is temporarily stopped. Keep a detailed symptom journal noting when tinnitus or dizziness occurs relative to medication schedules, as some drugs cause immediate effects while others produce symptoms only after cumulative exposure. Always consult with your healthcare provider before adjusting or discontinuing any prescription medication, as sudden cessation can sometimes cause additional problems or rebound effects. For more information on managing tinnitus, you can explore best drugs for tinnitus options reviewed by experts.
If you suspect a medication may be contributing to your symptoms, ask your doctor about monitoring options such as audiological testing or vestibular evaluation to track potential changes over time. In many cases, alternative medications with lower ototoxicity risk may be available, or dosage adjustments can minimize side effects while maintaining therapeutic benefits. Remember that individual sensitivity to medication-induced ear effects varies significantly based on genetic factors, pre-existing conditions, and other medications you may be taking concurrently.
When to See a Doctor: Red Flag Symptoms
“tinnitus patients” from www.healthyhearing.com and used with no modifications.
Warning Signs Requiring Immediate Medical Attention
- Sudden, severe vertigo with hearing loss in one ear (possible labyrinthitis or stroke)
- Tinnitus and dizziness accompanied by facial weakness or numbness
- New-onset symptoms following head trauma
- Symptoms accompanied by severe headache, vision changes, or speech difficulties
- Progressive hearing loss with unilateral tinnitus and balance problems (possible acoustic neuroma)
While most cases of combined tinnitus and dizziness stem from benign conditions, certain patterns warrant prompt medical evaluation. Symptoms that appear suddenly and severely, particularly when accompanied by neurological changes like facial weakness, visual disturbances, or coordination problems, could indicate serious conditions like stroke, multiple sclerosis, or other central nervous system disorders. Similarly, symptoms that consistently worsen over time despite conservative measures suggest potentially progressive conditions requiring intervention.
The timing and context of symptoms provide important diagnostic clues. Episodic symptoms that occur in defined attacks, like those in Ménière’s disease or vestibular migraine, typically follow different treatment pathways than constant symptoms that suggest structural problems. Healthcare providers will particularly note whether symptoms are unilateral (affecting one ear) or bilateral, as one-sided symptoms sometimes indicate more concerning conditions requiring imaging or specialized testing.
Don’t hesitate to seek emergency care if dizziness is severe enough to prevent walking or is accompanied by symptoms like chest pain, shortness of breath, or severe headache described as “the worst headache of your life.” These combinations may indicate life-threatening conditions requiring immediate attention. Remember that early diagnosis of conditions causing tinnitus and dizziness often leads to more effective treatment and better outcomes, making timely medical consultation essential for persistent or concerning symptoms.
Emergency Warning Signs
Certain combinations of symptoms require immediate medical attention. Seek emergency care if you experience sudden, severe vertigo accompanied by hearing loss, especially if it occurs with other neurological symptoms like facial weakness, slurred speech, or inability to walk. These could indicate a stroke affecting the brain stem or inner ear blood supply. Similarly, new tinnitus and dizziness following head trauma, accompanied by confusion, worsening headache, or clear fluid from the ears or nose might signal a skull fracture or brain injury requiring urgent evaluation.
Tests Your Doctor Will Likely Order
Diagnosing the cause of concurrent tinnitus and dizziness typically involves a series of specialized tests. Audiometric testing evaluates hearing function, while videonystagmography (VNG) assesses vestibular system responses to different stimuli. Your doctor may also order vestibular evoked myogenic potentials (VEMP) to check specific vestibular pathways, or rotary chair testing to evaluate how well your eyes and inner ears work together during movement.
Imaging studies often play a crucial role in diagnosis, with MRI being particularly valuable for visualizing the inner ear structures, vestibulocochlear nerve, and brain. In some cases, specialized CT scans help identify bony abnormalities like superior canal dehiscence. Blood tests might be ordered to check for systemic conditions like autoimmune disorders, vitamin deficiencies, or thyroid dysfunction that can contribute to both symptoms. Your doctor will select the most appropriate tests based on your specific symptom pattern and medical history.
Frequently Asked Questions
Living with tinnitus and dizziness generates many questions about causes, connections, and coping strategies. The following responses address common concerns and misconceptions about these interrelated symptoms, providing evidence-based information to help you better understand and manage your condition.
Remember that while these general answers apply to many situations, your specific experience may vary based on your unique health circumstances. Always consult with healthcare professionals for personalized advice related to your symptoms.
Can anxiety make tinnitus and dizziness worse?
Yes, anxiety can significantly amplify both tinnitus and dizziness symptoms through several mechanisms. When anxious, your body releases stress hormones that can increase blood pressure, muscle tension, and sensory sensitivity—all of which can intensify tinnitus perception. Similarly, anxiety often triggers hyperventilation and changes in autonomic nervous system function that contribute to lightheadedness and unsteadiness. Many patients describe entering a “feedback loop” where tinnitus or dizziness creates anxiety, which then worsens the original symptoms.
Research published in the Journal of Psychosomatic Research found that psychological interventions targeting anxiety, such as cognitive-behavioral therapy, significantly reduced tinnitus distress in 75% of study participants, with many also reporting improvements in associated dizziness. For maximum symptom relief, comprehensive treatment approaches often combine traditional medical interventions with anxiety-management strategies like mindfulness meditation, progressive muscle relaxation, and breathing exercises specifically designed to calm the autonomic nervous system.
Is it possible to have tinnitus without hearing loss?
Absolutely. While tinnitus and hearing loss frequently occur together, many people experience tinnitus despite having normal hearing on standard audiometric tests. This “normal-hearing tinnitus” accounts for approximately 10-15% of all tinnitus cases. In these situations, the tinnitus may result from subtle cochlear damage that doesn’t yet affect hearing thresholds, alterations in central auditory processing, or problems in non-auditory brain regions that influence sound perception.
Interestingly, research using specialized testing often reveals subtle hearing abnormalities in people with seemingly normal hearing and tinnitus. Advanced techniques like high-frequency audiometry and speech-in-noise testing can detect early auditory system changes before they’re apparent on standard hearing tests. This suggests that while clinically normal hearing with tinnitus is possible, truly unaffected auditory function with tinnitus is relatively rare.
Normal-hearing tinnitus appears more common in younger individuals and those whose tinnitus stems from temporomandibular joint (TMJ) disorders, certain medications, or stress-related factors. It’s worth noting that even without current hearing loss, people with tinnitus may have an increased risk of developing hearing problems later, making hearing conservation and regular monitoring important preventative measures.
If you have tinnitus without apparent hearing loss, a thorough evaluation remains important to identify potential underlying causes and establish baseline measurements for future comparison. This should include comprehensive audiometric testing, detailed medical history review, and possibly specialized tests to evaluate vestibular function if dizziness is also present.
- Somatosensory tinnitus (related to neck or jaw problems) often occurs without hearing loss
- Pulsatile tinnitus (synchronized with heartbeat) frequently presents with normal hearing
- Medication-induced tinnitus can develop before detectable hearing changes
- Stress-related tinnitus commonly appears despite normal audiograms
- Post-traumatic tinnitus sometimes occurs after head injury without affecting hearing thresholds
How long does dizziness from tinnitus typically last?
The duration of dizziness associated with tinnitus varies widely depending on the underlying cause. In Ménière’s disease, vertigo attacks typically last 20 minutes to several hours, while vestibular migraine episodes may persist for minutes to days. BPPV causes brief dizziness lasting seconds to minutes with specific head positions. Medication-related dizziness often continues until the drug is metabolized or discontinued. Rather than tinnitus directly causing dizziness, both symptoms usually stem from the same underlying condition, with their timing and duration determined by that specific disorder. Tracking your symptom patterns provides valuable diagnostic information for your healthcare provider.
Can diet changes help reduce tinnitus and dizziness symptoms?
Dietary modifications can indeed influence both tinnitus and dizziness symptoms in many individuals. Research particularly supports limiting sodium intake for those with Ménière’s disease, as high salt consumption can alter inner ear fluid pressure. Similarly, reducing caffeine, alcohol, and artificial sweeteners benefits many patients, as these substances can affect inner ear blood flow and neural excitability. Tyramine-rich foods (aged cheeses, processed meats, fermented foods) and those containing MSG may trigger vestibular migraines in susceptible individuals. While no universal “tinnitus diet” exists, keeping a food journal to identify personal triggers, maintaining stable blood sugar levels, and ensuring adequate hydration can significantly improve symptom management for many people struggling with both tinnitus and dizziness.
Are tinnitus and dizziness symptoms of something more serious?
While most cases of combined tinnitus and dizziness stem from benign inner ear conditions, these symptoms occasionally signal more serious underlying issues. Acoustic neuromas (vestibular schwannomas), though rare, typically present with progressive unilateral tinnitus, hearing loss, and balance problems. Multiple sclerosis sometimes manifests with both symptoms, particularly when lesions affect the brainstem or cranial nerve pathways. Rarely, conditions affecting cerebrospinal fluid pressure or cerebrovascular abnormalities can produce both tinnitus and dizziness. The pattern, progression, and accompanying symptoms provide critical diagnostic clues—sudden onset of severe symptoms, particularly with neurological changes like facial numbness or visual disturbances, warrants immediate medical evaluation.
If you’re experiencing persistent or recurrent episodes of both tinnitus and dizziness, a thorough evaluation by an ear specialist (otolaryngologist) or neurotologist is recommended. These specialists can distinguish between common, benign causes and more concerning conditions through comprehensive testing and clinical assessment. Most patients ultimately receive reassuring diagnoses of manageable inner ear or vestibular disorders, but proper evaluation provides both peace of mind and appropriate treatment direction.