Key Takeaways
- Tinnitus is the perception of sound (like ringing or buzzing) when no external noise is present, affecting an estimated 10-25% of American adults.
- While often described as “ringing in the ears,” tinnitus can manifest as buzzing, humming, clicking, roaring, or whistling sounds that vary in pitch and intensity.
- Most cases of tinnitus are subjective (only heard by the affected person) and commonly associated with hearing loss, though many other causes exist.
- Pittsburgh Audiology specialists can help diagnose and develop personalized management strategies for those struggling with persistent tinnitus symptoms.
- Understanding the type, pattern, and triggers of your tinnitus is essential for proper diagnosis and finding effective relief strategies.
What Is Tinnitus? Understanding the Phantom Sounds in Your Ears
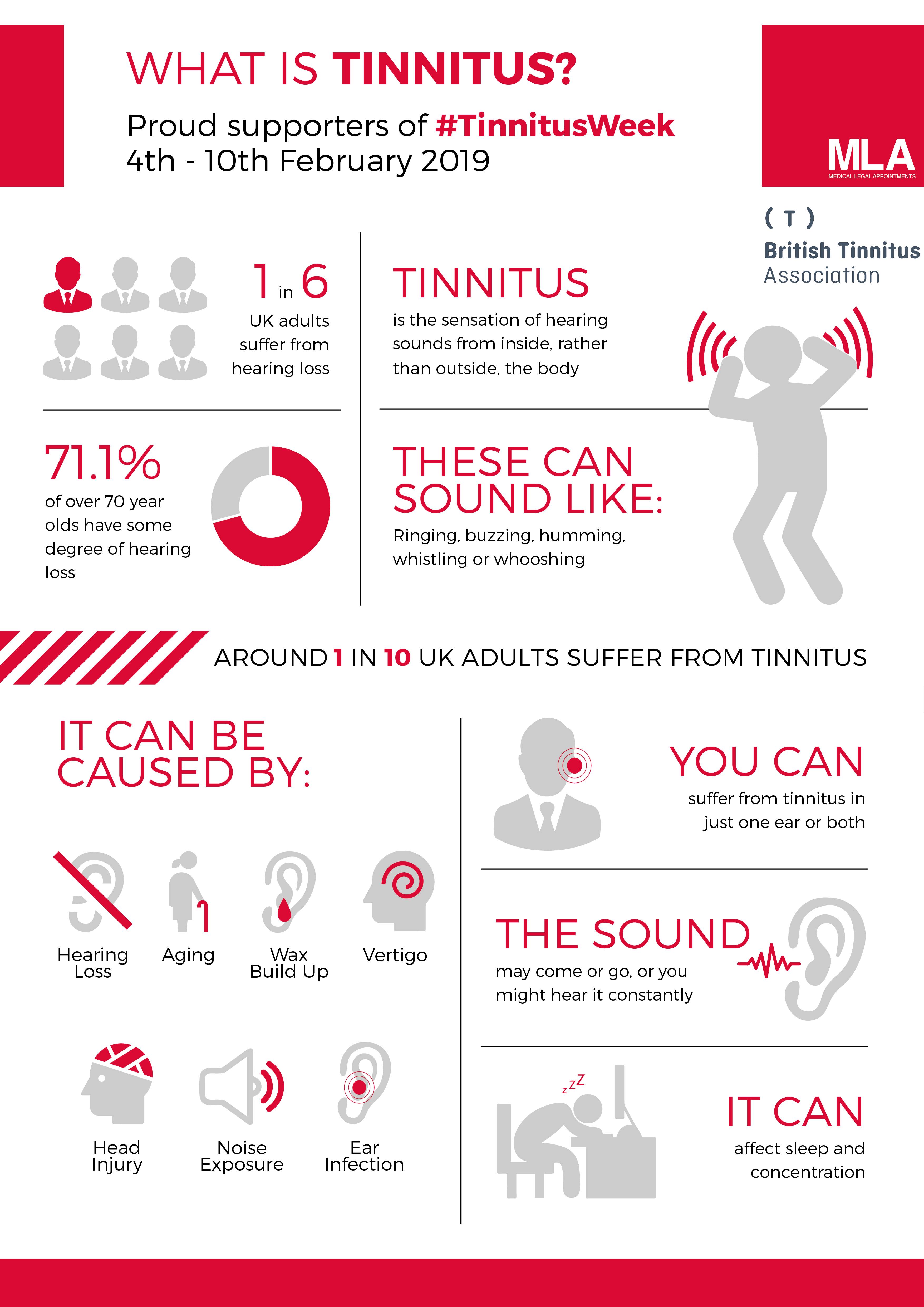
“What is Tinnitus? | Infographic” from www.mla-ltd.co.uk and used with no modifications.
That persistent ringing in your ears has a name: tinnitus. Pronounced either “tih-NIGHT-us” or “TIN-ih-tus,” this condition affects over 50 million Americans who experience some degree of phantom sounds that others cannot hear. Tinnitus isn’t actually a disease but rather a symptom that something else may be happening with your auditory system. Think of it as your ears and brain creating sound when no external sound source exists—similar to a phantom limb sensation, but for your hearing. Pittsburgh Audiology specialists regularly work with patients trying to understand and manage these persistent sounds that can range from mildly annoying to severely disruptive.
What makes tinnitus particularly challenging is its subjective nature—the experience varies dramatically between individuals. For some, it’s a faint background noise that’s only noticeable in quiet rooms. For others, it can be loud enough to interfere with concentration, sleep, and daily activities. About 20 million Americans experience persistent tinnitus that significantly impacts their quality of life, while millions more notice it occasionally.
Understanding tinnitus begins with recognizing that while the sensation seems to come from your ears, the phantom sounds are actually generated by your brain in an area called the auditory cortex. This often happens when damage to the inner ear changes the signals carried by nerves to the sound-processing parts of your brain. Rather than a malfunction of the ear itself, tinnitus represents your brain’s response to altered auditory input—a crucial distinction that helps explain why treatment approaches focus on both the ear and the brain.
The Different Sounds of Tinnitus
“Tinnitus Symptoms: Common Sounds of Ear …” from www.healthyhearing.com and used with no modifications.
Tinnitus manifests in remarkably diverse ways, which can sometimes make it difficult to recognize or describe to healthcare providers. While “ringing in the ears” is the common shorthand description, this simplification doesn’t capture the wide spectrum of sounds that tinnitus sufferers actually experience. Understanding the specific characteristics of your tinnitus—including the sound type, pitch, volume, and pattern—can help healthcare professionals better diagnose and treat your condition.
Ringing, Buzzing, and Humming Sensations
The classic high-pitched ringing is perhaps the most frequently reported form of tinnitus, resembling the sound after exposure to loud noise or the tone of an old television that’s been left on. However, many people describe their tinnitus as more of a buzzing sensation, similar to electrical interference or the sound of insects. Others experience humming tones that can be low, medium, or high in pitch—sometimes even resembling musical notes or tones. For those looking to manage their symptoms, sound therapy offers expert insights on relief strategies.
The quality of these sounds often provides clues about potential causes. High-pitched ringing or buzzing frequently correlates with noise-induced hearing loss or age-related hearing changes affecting the high-frequency detecting hair cells in your inner ear. Lower-pitched humming might suggest different underlying factors, potentially related to blood flow or muscle contractions near the ear.
When Tinnitus Sounds Like Clicking or Pulsating
- Clicking or crackling sounds that occur in patterns, often when swallowing or moving your jaw, may indicate Eustachian tube dysfunction or temporomandibular joint (TMJ) issues
- Pulsatile tinnitus—sounds that beat in rhythm with your pulse—warrants special medical attention as it can relate to blood vessel conditions near the ear
- Whooshing sounds synchronized with heartbeats sometimes indicate objective tinnitus, which doctors may actually be able to hear with specialized equipment
- Clicking that occurs in regular patterns might stem from muscle spasms in the middle ear
These rhythmic forms of tinnitus differ significantly from the constant sounds most commonly experienced. Pulsatile tinnitus in particular deserves prompt medical evaluation, as it sometimes indicates vascular abnormalities that require treatment. If you notice your tinnitus matches your heartbeat or changes when you exercise, lie down, or turn your head, be sure to mention these specific patterns to your healthcare provider.
One Ear vs. Both Ears: How Tinnitus Varies
Tinnitus can occur in just one ear (unilateral), both ears (bilateral), or seem centered somewhere in your head rather than specifically in either ear. These location differences matter significantly for diagnosis. Unilateral tinnitus—especially when accompanied by hearing loss on the same side—requires thorough investigation as it occasionally indicates structural problems like acoustic neuromas (benign tumors on the hearing nerve). Bilateral tinnitus more commonly relates to widespread hearing damage from noise exposure, aging, or certain medications affecting both ears.
The perceived location can shift over time, with some people reporting tinnitus that moves from one ear to both, or seems to travel across their head. The intensity and character may also fluctuate throughout the day or in response to environmental factors like background noise, stress levels, or even caffeine consumption. Keeping a tinnitus journal tracking these patterns can provide valuable information for healthcare providers working to identify triggers and effective management strategies for your specific type of tinnitus.
Common Causes Behind the Ringing
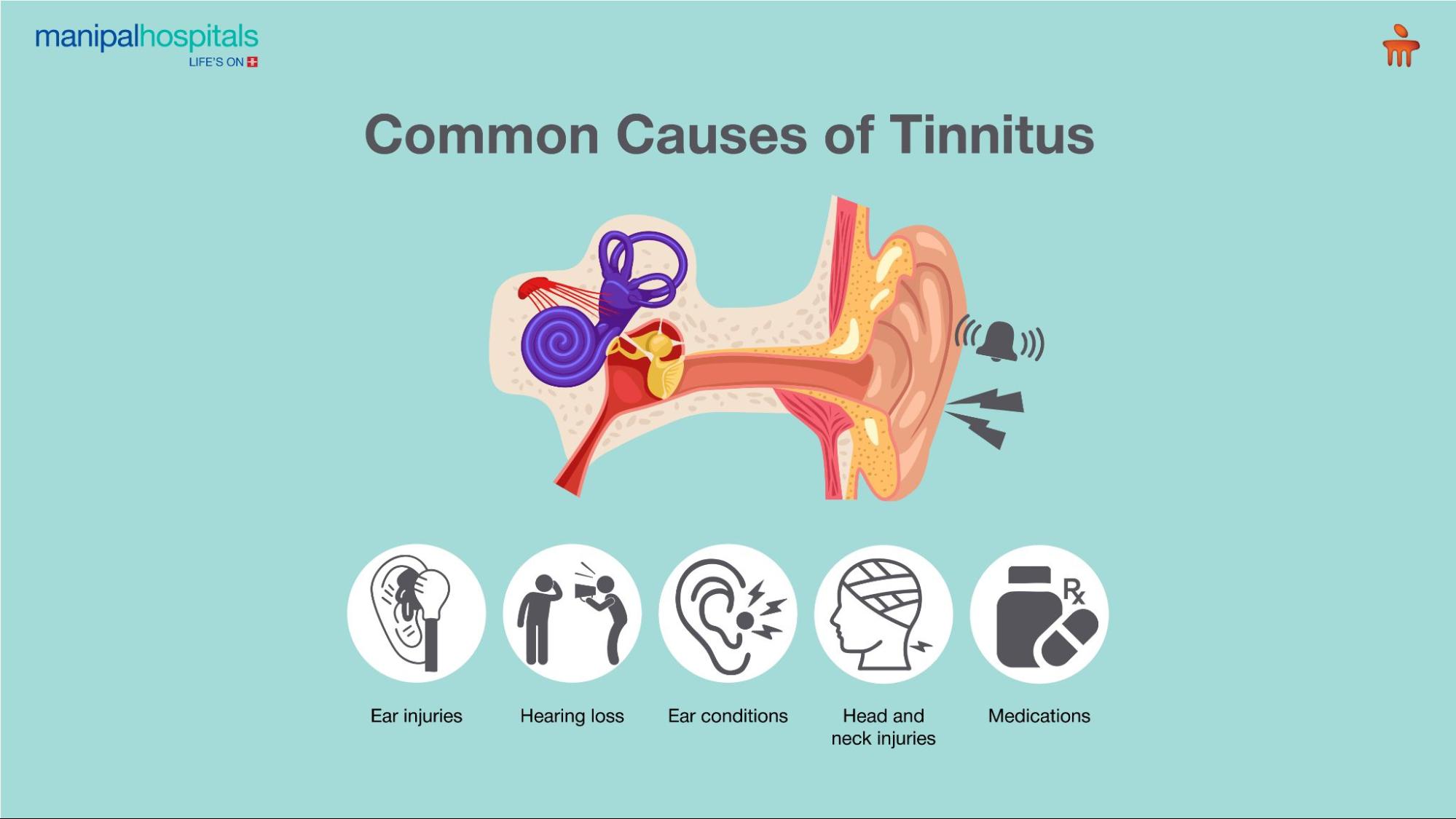
“Understanding Tinnitus: Causes …” from www.manipalhospitals.com and used with no modifications.
Understanding what triggers tinnitus is crucial for both treatment and peace of mind. While the exact mechanisms aren’t fully understood in every case, several common factors have been consistently linked to the development of tinnitus symptoms. Identifying the underlying cause can significantly impact treatment approaches and help prevent worsening of symptoms over time.
The relationship between hearing loss and tinnitus is particularly strong, with an estimated 90% of tinnitus cases occurring alongside some degree of hearing impairment. This connection explains why hearing aids and other hearing interventions often provide relief for tinnitus sufferers—by amplifying external sounds, they help mask the internal phantom sounds and give the brain more appropriate auditory stimulation.
Hearing Loss and Its Connection to Tinnitus
Hearing loss is the single most common factor associated with tinnitus. When the delicate hair cells in your inner ear become damaged or deteriorate, they no longer transmit sound signals properly to your brain. This disruption in normal auditory input appears to trigger compensatory activity in the brain’s auditory processing centers, producing the phantom sounds of tinnitus. The relationship works both ways—tinnitus can be an early warning sign of hearing loss, while existing hearing loss often makes tinnitus more noticeable by reducing background sounds that would otherwise mask it.
The type and configuration of your hearing loss often correlates with your tinnitus experience. For instance, high-frequency hearing loss typically pairs with high-pitched tinnitus, while broader hearing loss patterns might produce more complex tinnitus sounds. This is why audiologists measure your hearing function across different frequencies—the pattern of hearing loss provides valuable clues about your tinnitus and how best to address it.
Age-Related Factors That Trigger Tinnitus
As we age, our risk for developing tinnitus increases significantly. This is largely due to age-related hearing loss (presbycusis), which affects roughly one-third of adults over age 65. The gradual deterioration of inner ear structures occurs naturally with aging, but the process can be accelerated by other factors like noise exposure or certain health conditions. Beyond hearing changes, age-related stiffening of the middle ear bones and other structural alterations can contribute to tinnitus development in older adults.
Circulation problems more common in aging populations may also play a role in tinnitus, particularly the pulsatile variety. Changes in blood vessel elasticity or blood pressure regulation can alter blood flow near the ear, sometimes creating audible sounds. Additionally, the cumulative effect of medications taken for age-related conditions can impact tinnitus, with older adults more likely to be taking multiple prescriptions that might affect hearing function.
Noise Exposure Damage
Exposure to loud noise remains one of the most preventable causes of tinnitus. A single traumatic noise event (like an explosion or concert without hearing protection) or chronic exposure to noise levels above 85 decibels can permanently damage the delicate hair cells of your inner ear. This noise-induced hearing loss frequently leads to tinnitus that may appear immediately or develop gradually over time. Military personnel, construction workers, musicians, and factory workers face particularly high risks, though everyday exposures like lawn equipment, power tools, and even personal audio devices at high volumes can cause similar damage. For those affected, hearing aids with tinnitus features can offer significant relief.
The insidious nature of noise damage often means people don’t realize the harm until tinnitus or hearing problems become noticeable. The damage accumulates silently over years, with each exposure potentially contributing to the eventual development of symptoms. This underscores the importance of hearing protection in noisy environments, even when the noise seems temporarily tolerable.
Medications That Can Cause Tinnitus
Over 200 medications list tinnitus as a potential side effect, with certain drug classes posing particularly high risks. Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) can cause temporary tinnitus at high doses, while certain antibiotics (especially aminoglycosides like gentamicin), cancer medications (cisplatin and others), and diuretics (particularly loop diuretics like furosemide) may cause permanent hearing damage and tinnitus. The relationship between medications and tinnitus is often dose-dependent, with higher doses or longer treatment durations increasing the risk. For those seeking relief, tinnitus patches have been explored as a potential solution.
Never stop taking prescribed medications without consulting your healthcare provider, even if you suspect they’re contributing to your tinnitus. Instead, discuss your concerns with your doctor, who may be able to adjust dosages, switch to alternative medications, or help implement strategies to manage the tinnitus while continuing necessary treatments. Always report new or worsening tinnitus when starting new medications so potential connections can be identified early.
Medical Conditions Associated With Ear Ringing
Beyond hearing-specific issues, numerous medical conditions can trigger or worsen tinnitus. Temporomandibular joint (TMJ) disorders affect the jaw joint near the ear and frequently cause tinnitus that varies with jaw movement. Head and neck injuries, particularly those involving concussion or whiplash, can damage auditory pathways and lead to persistent tinnitus. Metabolic disorders like diabetes, thyroid dysfunction, and vitamin deficiencies may create biochemical conditions that impact auditory function. For more insights on relief strategies, you can explore tinnitus treatment options.
Cardiovascular conditions deserve special attention regarding tinnitus. High blood pressure, atherosclerosis (hardening of the arteries), and abnormal blood vessel formations near the ear can all produce pulsatile tinnitus—sounds that match your heartbeat. These cases often represent objective tinnitus that healthcare providers can actually detect with proper equipment, distinguishing them from the more common subjective forms that only the patient can perceive.
Rarely, tinnitus may signal serious conditions like Meniere’s disease (characterized by episodes of vertigo, fluctuating hearing loss, and tinnitus), acoustic neuromas (benign tumors on the hearing nerve), or other growths affecting the ear or auditory pathways. While these conditions are uncommon, they highlight the importance of thorough medical evaluation for persistent or worsening tinnitus, particularly when it occurs only in one ear or alongside other symptoms like dizziness, facial numbness, or rapid hearing changes.
Subjective vs. Objective Tinnitus: Critical Differences
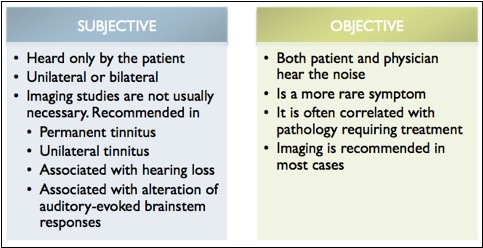
“EPOS™” from epos.myesr.org and used with no modifications.
The distinction between subjective and objective tinnitus represents a fundamental classification that guides both diagnosis and treatment approaches. Understanding which category your tinnitus falls into helps determine appropriate medical specialists, necessary testing, and potential treatment options. While the symptoms may feel similar to the person experiencing them, the underlying mechanisms differ significantly.
Medical professionals use this classification as a first step in evaluation, as it immediately narrows down potential causes and points toward specific diagnostic pathways. The treatment success rates also vary between these categories, with objective tinnitus often more responsive to direct medical or surgical interventions targeting the identified sound source.
Subjective Tinnitus: When Only You Hear It
Subjective tinnitus accounts for approximately 95% of all tinnitus cases and is defined by sounds that only the affected individual can hear. This form originates from neural activity in the auditory system and represents the brain’s response to altered or missing input from the ear. When hair cells in the inner ear become damaged or deteriorate, they send abnormal signals (or stop sending signals altogether) to the brain, which may respond by generating phantom sounds as it attempts to compensate for the missing information. The resulting tinnitus can vary tremendously in character, volume, and impact on quality of life.
What makes subjective tinnitus particularly challenging is that it cannot be measured objectively by current medical technology. There’s no test that can detect the sound or quantify its intensity—healthcare providers must rely entirely on the patient’s description. Despite this limitation, subjective tinnitus is very real and can be validated through specialized questionnaires that assess its impact, specialized hearing tests that may match the tinnitus pitch, and brain imaging studies that show altered activity in auditory processing centers during tinnitus episodes.
Common causes of subjective tinnitus include sensorineural hearing loss (from aging, noise exposure, or other factors), ototoxic medications, ear infections, impacted earwax, and Meniere’s disease. Management typically focuses on addressing any underlying conditions, using sound therapy to mask the tinnitus, and cognitive behavioral approaches that help reduce awareness of and distress from the sounds.
Objective Tinnitus: When Doctors Can Detect It
In stark contrast to subjective tinnitus, objective tinnitus produces sounds that can potentially be heard by someone other than the affected person. These sounds typically originate from physical structures near the ear rather than from neural activity, and they represent actual acoustic events happening within or around the auditory system. A healthcare provider may be able to detect these sounds using a stethoscope or specialized microphones placed in or near the ear canal. This detectability makes objective tinnitus somewhat easier to diagnose and often more responsive to direct treatment of the underlying cause.
The most common form is pulsatile tinnitus, where the sound synchronizes with the heartbeat due to blood flow disturbances. Causes include abnormal blood vessels near the ear, increased awareness of normal blood flow (often due to conductive hearing loss), high blood pressure, and vascular tumors. Another form involves rhythmic clicking or crackling from muscle contractions—middle ear muscle spasms or palatal myoclonus can create regular clicking sensations that others might hear with proper equipment.
Key Difference: Treatment Approach
While subjective tinnitus often requires multifaceted management strategies focused on perception and coping, objective tinnitus may be completely curable if the physical source can be identified and addressed. For instance, surgically correcting an abnormal blood vessel or treating high blood pressure might completely resolve pulsatile tinnitus, while muscle relaxants might stop myoclonic clicking.
How Doctors Diagnose Tinnitus
“How Is Tinnitus Diagnosed? – YouTube” from www.youtube.com and used with no modifications.
Diagnosing tinnitus goes beyond simply confirming that you hear phantom sounds—it involves identifying patterns, potential causes, and associated conditions that might guide treatment. Since tinnitus is a symptom rather than a standalone condition, a thorough diagnostic process seeks to uncover any underlying factors that could be addressed directly. This multifaceted approach typically involves several healthcare professionals working together to build a complete picture of your condition.
Initial Evaluation by Primary Care Physicians
Your diagnostic journey typically begins with your primary care doctor, who will gather a comprehensive history of your tinnitus experience. They’ll ask detailed questions about when your tinnitus started, whether it’s constant or intermittent, how it sounds, and what seems to make it better or worse. Your doctor will also review your complete medical history, medication list, and any recent changes in health status that might correlate with tinnitus onset. This initial conversation provides crucial context for understanding potential causes.
A basic physical examination follows, with special attention to your ears, head, and neck. Your doctor will look for visible abnormalities like earwax blockage, eardrum perforations, or signs of infection that might explain your symptoms. They’ll also check for less obvious issues like TMJ dysfunction or neck problems that can sometimes trigger tinnitus. Based on these findings, they may initiate basic treatment (like earwax removal) or refer you to specialists for more comprehensive evaluation.
What to Expect at Your ENT Appointment
Otolaryngologists (ENTs) specialize in conditions affecting the ears, nose, and throat, making them key specialists in tinnitus diagnosis. At an ENT appointment, you’ll undergo a more detailed examination of your ear structures using specialized equipment like an otoscope. The doctor will evaluate your ear canal, eardrum, and sometimes the middle ear space for abnormalities. They may perform tests to check eardrum movement and middle ear function, which can reveal conditions like Eustachian tube dysfunction or otosclerosis that might contribute to tinnitus.
ENTs also assess cranial nerve function and conduct balance testing when appropriate, as some conditions causing tinnitus (like Meniere’s disease) also affect balance. For pulsatile tinnitus, they may listen with a stethoscope placed near your ear or neck to detect vascular sounds. When necessary, they’ll order specialized tests like CT scans or MRIs to examine structures around the ear in greater detail, particularly if they suspect tumors, vascular abnormalities, or other structural issues.
Audiologist Testing and Evaluation
Audiologists play a crucial role in tinnitus diagnosis through comprehensive hearing assessments. A complete audiological evaluation typically includes pure-tone audiometry to measure hearing thresholds across different frequencies, speech recognition testing to assess how well you understand spoken language, and impedance testing to evaluate middle ear function. These tests help determine whether hearing loss exists alongside your tinnitus and, if so, what type and severity—information that directly informs treatment recommendations.
Specialized tinnitus assessments may include tinnitus pitch and loudness matching, where the audiologist uses sound generators to create tones similar to what you’re experiencing. This helps characterize your tinnitus more precisely and establishes a baseline for monitoring changes over time. Minimum masking level testing determines how loud an external sound needs to be to cover or mask your tinnitus, information that guides sound therapy approaches. Some audiologists also use questionnaires like the Tinnitus Handicap Inventory to quantify how tinnitus affects your daily life, emotional well-being, and functionality.
Imaging Tests for Tinnitus Diagnosis
While not necessary for all tinnitus cases, imaging studies become important when certain patterns or associated symptoms raise concerns about underlying structural causes. MRI (Magnetic Resonance Imaging) provides detailed images of soft tissues, making it particularly valuable for examining the auditory nerve pathway and brain structures involved in hearing. It’s typically recommended for unilateral (one-sided) tinnitus, tinnitus accompanied by asymmetric hearing loss, or cases with neurological symptoms that might suggest tumors or other abnormalities affecting the hearing pathway.
CT (Computed Tomography) scans offer superior visualization of bony structures and can help identify abnormalities in the temporal bone surrounding the ear or calcifications that might affect hearing. For pulsatile tinnitus, specialized vascular imaging like CT angiography or MR angiography may be ordered to examine blood vessels around the ear and brain. These studies can reveal abnormalities like stenosis (narrowing), malformations, or tumors affecting blood flow near the auditory system.
Children and Tinnitus: Special Considerations
“When Your Child Has Tinnitus | Dubuque ENT” from dubuqueent.com and used with no modifications.
While often considered an adult condition, tinnitus affects children more frequently than many realize. Research suggests that up to 35% of children may experience tinnitus at some point, though they’re less likely to report it spontaneously unless specifically asked. Children process and communicate about sensory experiences differently than adults, making pediatric tinnitus particularly challenging to identify and address. The impact on learning, attention, and emotional development can be significant when tinnitus goes unrecognized in young people.
Signs Your Child May Have Tinnitus
Children rarely use terms like “ringing” or “tinnitus” to describe their experiences, instead using more concrete descriptions or behavioral indicators. They might cover their ears in quiet environments, ask to have music or television on constantly, or complain that their ears feel “funny” or “full.” Some children show increased irritability, difficulty concentrating, or sleep disturbances that seem unexplained. School performance might decline, particularly for tasks requiring sustained attention in quiet settings.
Younger children may not recognize that hearing phantom sounds is unusual, assuming everyone experiences the same sensations. They might become anxious in quiet environments or develop behaviors to cope with or mask the sounds, like humming to themselves or seeking constant background noise. Parents should be particularly alert if their child has risk factors like recent ear infections, exposure to loud noise (including through headphones), or family history of hearing problems.
Helping Children Cope With Ear Ringing
Managing tinnitus in children follows many of the same principles as adult treatment but requires age-appropriate adaptations. Explaining tinnitus in simple, non-threatening terms helps children understand what’s happening without becoming fearful. Sound therapy can be particularly effective, with gentle background sounds like white noise machines at bedtime or appropriate classroom accommodations that minimize quiet stress. For children with associated hearing loss, properly fitted hearing aids can address both issues simultaneously.
Involving school personnel ensures that children receive necessary support in learning environments. Simple accommodations like preferential seating, permission to use background music during independent work, or short breaks when tinnitus becomes distracting can significantly improve academic experiences. Cognitive behavioral strategies can be adapted for children, teaching them age-appropriate ways to shift attention away from the tinnitus and develop positive coping mechanisms.
Frequently Asked Questions
As patients begin to learn about tinnitus, certain questions consistently arise during consultations. These common concerns reflect the complex nature of tinnitus and the uncertainty many feel when first experiencing these phantom sounds. Understanding the answers to these questions provides a foundation for managing expectations and making informed decisions about care.
Can tinnitus go away on its own?
Many cases of temporary tinnitus do resolve spontaneously, particularly those triggered by short-term factors like ear infections, medication reactions, or brief noise exposure. After attending a loud concert, for example, you might experience ringing that fades within hours or days as your auditory system recovers. Similarly, tinnitus associated with earwax buildup or middle ear fluid typically disappears once these conditions are treated. However, tinnitus lasting longer than three months is considered chronic and less likely to resolve completely without intervention.
Even chronic tinnitus can become less noticeable over time through a process called habituation, where your brain gradually learns to classify the tinnitus sounds as unimportant background noise. This natural adaptation process explains why many long-term tinnitus patients report that their perception of and distress from the sounds diminishes over time, even when the acoustic characteristics remain unchanged. Various tinnitus management approaches aim to accelerate this natural habituation process.
Is tinnitus a sign of serious illness?
While tinnitus itself is not life-threatening, it occasionally indicates underlying conditions requiring medical attention. For most people, tinnitus stems from common causes like hearing loss, aging changes, or noise exposure that, while important to address, don’t represent medical emergencies. However, certain patterns warrant prompt evaluation—particularly unilateral (one-sided) tinnitus with associated hearing loss, tinnitus that begins suddenly and severely, or pulsatile tinnitus synchronized with your heartbeat.
In rare cases, tinnitus may be associated with acoustic neuromas (benign tumors on the hearing nerve), blood vessel abnormalities, or other structural issues that require specific treatments. However, these serious causes represent a small minority of cases. The primary approach should be appropriate medical evaluation to rule out concerning causes, followed by focused management of the tinnitus itself and any identified contributing factors.
Why does my tinnitus get worse at night?
Nighttime often brings a perfect storm of factors that make tinnitus more noticeable. The reduced environmental sounds in quiet bedrooms remove the natural masking that helps hide tinnitus during daytime activities. Without the distractions and engagement of daily tasks, your attention may naturally focus more on internal sensations, including tinnitus. Additionally, fatigue from the day can lower your tolerance for annoying stimuli, making the same level of tinnitus feel more bothersome than it might when you’re rested.
Practical solutions include using subtle background sounds like white noise machines, fans, or specialized tinnitus apps that provide consistent, non-distracting sound throughout the night. Establishing relaxation routines before bedtime can reduce stress-related tinnitus amplification, while maintaining consistent sleep schedules helps regulate body systems that might influence tinnitus perception. For some, slightly elevating the head during sleep improves circulation and reduces tinnitus associated with positional changes.
What foods should I avoid if I have tinnitus?
While no universal dietary triggers affect all tinnitus sufferers, certain substances influence tinnitus perception in many individuals. Caffeine tops the list of potential aggravators—found in coffee, many teas, chocolate, and some medications, it can increase tinnitus intensity through its effects on blood flow and neural excitability. Similarly, alcohol may temporarily worsen tinnitus by altering blood flow patterns and fluid balance in the inner ear. High-sodium foods can affect fluid regulation throughout the body, potentially increasing pressure in the inner ear that worsens tinnitus, particularly for those with Meniere’s disease.
Rather than following generic restrictions, consider keeping a food diary tracking tinnitus intensity alongside consumption patterns to identify your personal triggers. Some patients report benefits from reducing MSG, artificial sweeteners, or processed foods, though scientific evidence for these connections remains limited. Focus on maintaining stable blood sugar through regular, balanced meals, as significant fluctuations in blood glucose can sometimes influence tinnitus perception through their effects on energy metabolism in auditory processing centers.
Can stress make tinnitus worse?
The relationship between stress and tinnitus creates a challenging cycle for many sufferers. Physiologically, stress triggers your body’s fight-or-flight response, releasing hormones like adrenaline and cortisol that can affect blood flow, muscle tension, and neural activity throughout the body—including auditory pathways. Many patients report that periods of increased stress, anxiety, or fatigue correlate directly with tinnitus flare-ups, even when the underlying condition hasn’t changed. This stress-reactivity explains why tinnitus often worsens during difficult life events or in high-pressure situations.
Breaking this cycle requires addressing both the tinnitus itself and your response to stress. Relaxation techniques like deep breathing, progressive muscle relaxation, and mindfulness meditation can reduce the physiological stress response and help manage tinnitus perception. Regular exercise supports overall stress management while promoting healthy circulation, potentially reducing tinnitus reactivity. For significant stress-related tinnitus exacerbations, cognitive behavioral therapy specifically tailored for tinnitus has shown strong evidence for reducing both tinnitus distress and its impact on quality of life.
Understanding your tinnitus is the first step toward managing it effectively. While the phantom sounds may never completely disappear for everyone, proper education, medical care, and coping strategies can significantly reduce their impact on your daily life. Remember that you’re not alone in this experience—millions share similar challenges, and healthcare providers continue developing more effective approaches to tinnitus management.
For personalized evaluation of your tinnitus symptoms and comprehensive treatment options, Pittsburgh Audiology specialists can develop a management plan tailored to your specific needs.