Key Takeaways
- Pulsatile tinnitus in one ear is a rhythmic sound synchronized with your heartbeat that may indicate underlying vascular or structural issues requiring medical attention.
- While many causes of unilateral pulsatile tinnitus are benign, some can indicate serious conditions like arteriovenous malformations or carotid artery disease that require immediate medical intervention.
- Unlike bilateral non-pulsatile tinnitus, one-sided pulsatile tinnitus warrants a thorough diagnostic workup including specialized imaging to identify potentially dangerous vascular abnormalities.
- The most common causes include venous sinus stenosis, carotid artery disease, and high-riding jugular bulbs, all of which can be effectively treated once properly diagnosed.
- Hearing a rhythmic whooshing sound in one ear that matches your pulse requires evaluation by an otolaryngologist, especially if accompanied by headaches, vision changes, or neurological symptoms.
What Is Pulsatile Tinnitus and Why It Happens in One Ear
“Pulsatile Tinnitus: 7 Different …” from www.youtube.com and used with no modifications.
That rhythmic whooshing or pulsing sound you hear in one ear that synchronizes perfectly with your heartbeat isn’t your imagination—it’s pulsatile tinnitus. Unlike the more common constant ringing tinnitus, pulsatile tinnitus has a distinct rhythmic quality that directly corresponds to your pulse. When experienced in just one ear, it often points to a localized issue affecting the blood vessels or structures near that specific ear.
Pulsatile tinnitus occurs in approximately 4% of people who seek medical attention for tinnitus problems, making it relatively uncommon but significant. The sound you’re hearing is actually turbulent blood flow through vessels near your ear canal. Think of it like putting your ear against a garden hose with water rushing through it—any narrowing, bulging, or irregular pathways in that hose would create distinctive sounds. In your case, those sounds are happening inside your head, specifically near one ear.
What makes one-sided pulsatile tinnitus particularly noteworthy is that it frequently indicates an underlying anatomical or vascular abnormality that requires medical attention. While regular bilateral tinnitus is often benign, pulsatile tinnitus in a single ear could be your body’s warning system alerting you to potentially serious conditions that affect blood flow near that ear. The good news is that many causes of pulsatile tinnitus are identifiable and treatable with today’s advanced diagnostic techniques and targeted interventions.
Vascular Causes: Blood Vessel Problems Behind the Beating Sound
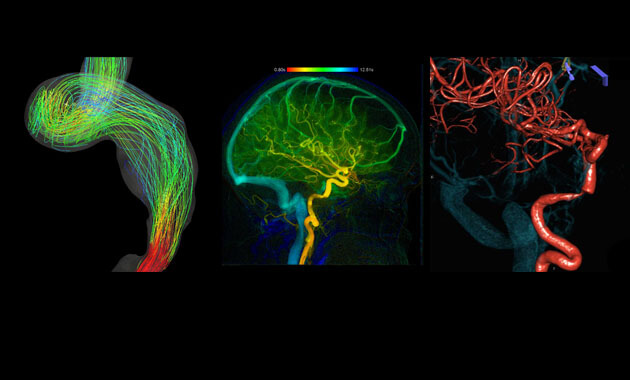
“Pulsatile Tinnitus Causes and …” from radiology.ucsf.edu and used with no modifications.
The majority of pulsatile tinnitus cases stem from vascular issues—problems with the blood vessels in or around your ear. When blood doesn’t flow smoothly through these vessels, it creates turbulence that you perceive as a rhythmic sound. This is especially noticeable in the quiet of night or in environments with minimal background noise. Vascular causes are particularly important to identify because some require immediate medical intervention to prevent serious complications like stroke or hearing loss.
Carotid Artery Abnormalities
Your carotid arteries—the major blood vessels supplying your brain with oxygenated blood—run very close to your ears. When these vital pathways develop problems, one-sided pulsatile tinnitus often results. Carotid artery stenosis, a narrowing due to plaque buildup, creates turbulent blood flow that produces the pulsing sound you hear. This condition typically affects adults in their 40s and 50s, particularly those with cardiovascular risk factors like smoking, high cholesterol, or diabetes.
Another carotid abnormality is fibromuscular dysplasia, a condition where the artery walls develop an irregular growth pattern creating a “string of beads” appearance. This genetic condition predominantly affects women and can cause sections of narrowing and widening that disrupt normal blood flow. Carotid artery dissection—a tear in the inner lining of the artery—is a more urgent condition that can also manifest as pulsatile tinnitus in one ear, often accompanied by facial or neck pain, headaches, or visual disturbances.
Jugular Vein Irregularities
While arteries carry blood away from your heart, veins return it, and problems with the jugular veins—the major vessels draining blood from your brain—can also cause one-sided pulsatile tinnitus. Jugular vein stenosis (narrowing) creates turbulent blood flow that you may hear as pulsing in your affected ear. Unlike arterial causes, venous pulsatile tinnitus may temporarily disappear when you press gently on your neck or turn your head to a certain position.
- Jugular vein thrombosis (blood clots)
- Jugular vein ectasia (abnormal dilation)
- Incomplete jugular vein valve closure
- Anatomical variants affecting normal venous drainage
The connection between these venous abnormalities and your ear lies in their proximity to your temporal bone and the intricate network of smaller veins that drain into the jugular system. When blood encounters resistance or irregular pathways in these structures, the turbulent flow creates sound waves that reach your inner ear, manifesting as the pulsatile tinnitus you experience.
Arteriovenous Malformations and Fistulas
Among the most serious vascular causes of pulsatile tinnitus in one ear are arteriovenous malformations (AVMs) and dural arteriovenous fistulas (DAVFs). These abnormal connections between arteries and veins bypass the normal capillary network, creating high-pressure, turbulent blood flow that generates the pulsating sound. DAVFs are particularly dangerous causes of pulsatile tinnitus and may develop following trauma, surgery, or infections, or sometimes spontaneously. The abnormal connection creates a “short circuit” in blood flow that not only produces distinctive sounds but can potentially lead to intracranial hemorrhage if left untreated.
The severity of symptoms typically correlates with the size and location of the malformation. Smaller AVMs might only produce the pulsatile tinnitus, while larger ones can cause additional symptoms including headaches, dizziness, or even neurological deficits. What makes these conditions particularly concerning is their potential to rupture, which represents a medical emergency requiring immediate intervention. If you experience sudden changes in your pulsatile tinnitus along with severe headache, vision changes, or weakness, seek emergency care immediately.
Turbulent Blood Flow From Atherosclerosis
Atherosclerosis—the buildup of fatty plaque in your arteries—is a common condition that can lead to pulsatile tinnitus in one ear. As plaque accumulates along the carotid artery wall, it narrows the passage through which blood flows, creating turbulence similar to water rushing through a partially blocked pipe. This turbulence generates sound waves that travel to your inner ear, manifesting as rhythmic pulsations synchronized with your heartbeat. The risk factors for atherosclerosis include high cholesterol, smoking, hypertension, diabetes, and family history of cardiovascular disease.
What makes atherosclerosis particularly concerning is that the pulsatile tinnitus might be an early warning sign of more serious vascular compromise. Beyond the annoying sound, the underlying arterial narrowing increases your risk of stroke and other cardiovascular events. Fortunately, addressing the underlying atherosclerosis through medication, lifestyle modifications, and sometimes surgical interventions can not only reduce your pulsatile tinnitus but also lower your risk of these more serious complications.
Pressure-Related Causes: When Fluid Builds Up
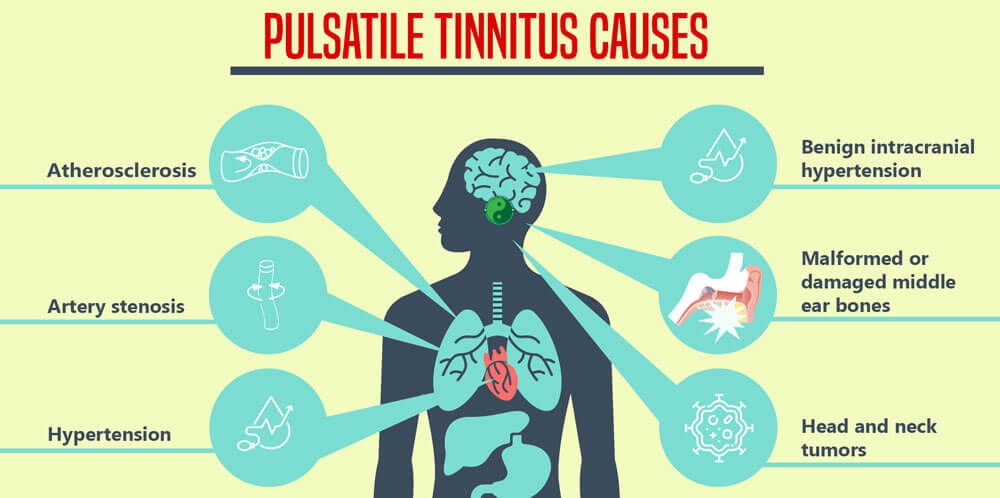
“Pulsatile Tinnitus – Philadelphia …” from philaholisticclinic.com and used with no modifications.
Not all causes of pulsatile tinnitus in one ear involve direct blood vessel abnormalities. Sometimes, the culprit is abnormal pressure that affects how you perceive normal blood flow. These pressure-related causes create conditions where the sound of your normal blood flow becomes audible, even though the vessels themselves may be structurally normal. Understanding these pressure dynamics helps explain why some people experience pulsatile tinnitus without having significant vascular malformations. For those seeking relief, exploring quick relief tips can be beneficial.
Benign Intracranial Hypertension (Pseudotumor Cerebri)
Benign intracranial hypertension (BIH), also called idiopathic intracranial hypertension or pseudotumor cerebri, is one of the most common causes of pulsatile tinnitus, particularly in young, overweight women. Despite its name including “benign,” this condition involves increased pressure of the cerebrospinal fluid surrounding your brain and can lead to serious complications if untreated. The elevated pressure compresses and alters the dynamics of venous blood flow, creating turbulence that manifests as pulsatile tinnitus, often predominantly in one ear.
Beyond the rhythmic sound in your ear, BIH frequently causes headaches, vision problems, and sometimes dizziness. The vision changes are particularly concerning, as untreated BIH can lead to permanent vision loss due to pressure on the optic nerve. Weight loss often helps reduce symptoms in overweight individuals, while medications like acetazolamide can help decrease cerebrospinal fluid production. In severe cases, surgical procedures to relieve the pressure may become necessary to preserve vision and reduce other symptoms, including the pulsatile tinnitus.
High Blood Pressure Effects on Ear Blood Vessels
Hypertension—chronically elevated blood pressure—can contribute to pulsatile tinnitus by increasing the force of blood flowing through vessels near your ear. The increased pressure makes normal blood flow more turbulent and thus more likely to generate audible sounds. Interestingly, this type of pulsatile tinnitus may affect just one ear if anatomical differences make one side more susceptible to picking up these sounds. Some patients report that their pulsatile tinnitus worsens during periods of stress or physical exertion when blood pressure temporarily rises even higher.
The good news about hypertension-related pulsatile tinnitus is that effectively controlling your blood pressure often reduces or eliminates the symptom. Lifestyle modifications like reducing sodium intake, regular exercise, stress management, and maintaining a healthy weight can make a significant difference. When these measures aren’t sufficient, anti-hypertensive medications prescribed by your doctor can help bring your blood pressure—and consequently your pulsatile tinnitus—under control.
Structural Abnormalities Leading to One-Sided Pulsatile Tinnitus
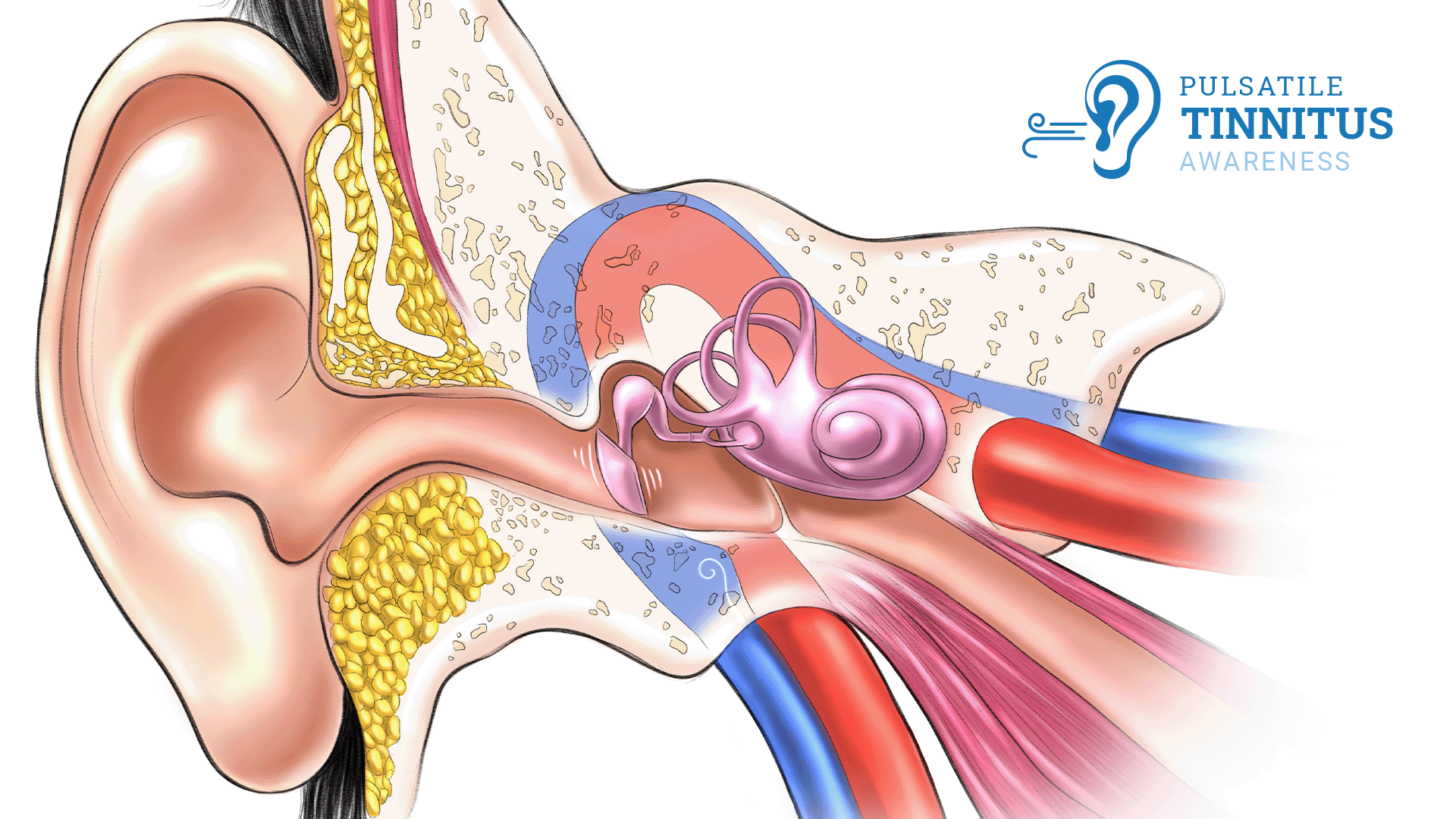
“Pulsatile Tinnitus Causes & Treatments” from www.neurosurgeonsofnewjersey.com and used with no modifications.
Sometimes the cause of pulsatile tinnitus in one ear isn’t the blood vessels themselves but the surrounding anatomical structures that influence how you perceive blood flow. These structural variations or abnormalities can amplify normal vascular sounds that would otherwise remain below your threshold of hearing. Understanding these structural causes helps explain why some people with normal vascular function still experience the rhythmic sounds of pulsatile tinnitus.
High-Riding Jugular Bulb
A high-riding jugular bulb occurs when the uppermost portion of the jugular vein—the jugular bulb—sits higher than normal in the temporal bone near your inner ear. This anatomical variant brings the pulsating blood flow closer to your hearing apparatus, making the normal sounds of venous return more audible. What makes this condition distinctive is that it’s often congenital (present from birth) rather than acquired, though you might not notice symptoms until adulthood when other factors like slight hearing loss make the pulsatile sound more prominent.
Diagnosis typically requires imaging studies like CT scans or MRI to visualize the relationship between your jugular bulb and temporal bone. If a high-riding jugular bulb is causing significant symptoms, surgical interventions to shield the bulb from your inner ear can sometimes help reduce the pulsatile tinnitus. However, many patients opt for non-surgical management strategies once they understand the benign nature of this anatomical variant and learn coping techniques for the symptoms.
Sigmoid Sinus Diverticulum and Dehiscence
Sigmoid sinus diverticulum occurs when part of the sigmoid sinus (a large vein inside your skull) bulges outward like a small balloon, while dehiscence happens when the bone that normally covers this blood vessel is abnormally thin or absent. Both conditions bring turbulent blood flow closer to your inner ear structures, creating the pulse-synchronized sounds you hear. What makes these conditions uniquely troublesome is that the altered blood flow patterns can create a persistent “whooshing” sound that becomes particularly noticeable in quiet environments or when you lie down with the affected ear against a pillow.
These structural abnormalities are actually quite treatable compared to some other causes of pulsatile tinnitus. Surgical repair of sigmoid sinus diverticulum or dehiscence has shown impressive success rates, with many patients experiencing complete resolution of their pulsatile tinnitus after the procedure. The surgery typically involves reinforcing the thin bone or reconstructing the affected area to buffer the sound of blood flow. Modern minimally invasive approaches have reduced recovery times and improved outcomes for patients undergoing these procedures.
Glomus Tumors and Other Vascular Growths
Glomus tumors (also called paragangliomas) are highly vascular growths that typically develop along blood vessels in your head and neck region. When these tumors form near your ear—such as glomus tympanicum in your middle ear or glomus jugulare near the jugular vein—they can cause persistent pulsatile tinnitus in the affected ear. These tumors are typically slow-growing and benign, but their rich blood supply creates the pulsing sound as blood flows through their abnormal vessel network. Women are more commonly affected, and there can be a genetic predisposition to developing these tumors.
Other vascular growths that may cause one-sided pulsatile tinnitus include hemangiomas and vascular malformations within the temporal bone. The diagnosis of these conditions typically requires specialized imaging studies including contrast-enhanced MRI or CT angiography. Treatment options range from watchful waiting for small, asymptomatic tumors to surgical removal, radiation therapy, or embolization procedures that cut off the tumor’s blood supply. The approach depends on the tumor’s size, location, growth rate, and the severity of your symptoms.
Non-Vascular Causes That Mimic Heart Rhythm in Your Ear
“Hearing Your Heartbeat in Only One Ear …” from www.myphteam.com and used with no modifications.
Not all pulsatile tinnitus stems from blood vessel issues. Sometimes, other structures near your ear can create rhythmic sounds that synchronize with your heartbeat or breathing. These non-vascular causes can be particularly confusing because they produce symptoms that mimic vascular pulsatile tinnitus but require entirely different treatment approaches. Understanding these alternative causes is crucial for proper diagnosis and management.
Middle Ear Muscle Spasms
Your middle ear contains two tiny muscles—the tensor tympani and stapedius—that normally contract in response to loud sounds to protect your inner ear. Sometimes these muscles can develop rhythmic, involuntary contractions that create a clicking or fluttering sensation synchronized with your pulse. Unlike true vascular pulsatile tinnitus, these muscle-related sounds might temporarily stop when you yawn, swallow, or change your jaw position. The condition, sometimes called middle ear myoclonus, can develop following ear infections, stress, or certain neurological conditions.
Treatment for middle ear muscle spasms may include muscle relaxants, anticonvulsant medications, or botulinum toxin injections in some cases. Stress reduction techniques can help when emotional factors trigger or worsen the spasms. For severe, treatment-resistant cases, surgical procedures to cut or weaken the affected muscle may be considered, though this is typically reserved as a last resort after less invasive approaches have failed. For additional insights on managing tinnitus, you might find it helpful to explore common tinnitus questions answered by a top audiologist.
Patulous Eustachian Tube
Your Eustachian tubes connect your middle ears to your throat, helping equalize pressure on both sides of your eardrums. A patulous (abnormally open) Eustachian tube fails to close properly, creating an open channel that allows sounds of your own breathing and blood flow to reach your middle ear. This condition often causes pulsatile tinnitus that synchronizes with your breathing rather than your heartbeat, though some patients report both respiratory and pulse-synchronized sounds. Weight loss, pregnancy, and certain medications can contribute to this condition by reducing the fatty tissue that normally helps keep the Eustachian tube closed. If you’re experiencing these symptoms, you might find it helpful to explore causes, relief, and treatments for buzzing in ears.
Many patients with patulous Eustachian tube find that simple maneuvers like lying down or tilting the head temporarily improve symptoms. Medical treatments include nasal estrogen sprays, saline nasal irrigation, or medications that promote fluid retention around the Eustachian tube. For persistent cases, surgical interventions to narrow the Eustachian tube opening or augment the surrounding tissue can provide relief. Unlike vascular causes of pulsatile tinnitus, patulous Eustachian tube is not dangerous but can significantly impact quality of life through its persistent, intrusive symptoms.
How Doctors Diagnose the True Cause of Your Pulsing Ear
“The Unwanted Beat of Pulsatile Tinnitus …” from www.pacificneuroscienceinstitute.org and used with no modifications.
Identifying the specific cause of pulsatile tinnitus in one ear requires a systematic diagnostic approach. Since the potential causes range from benign conditions to life-threatening vascular abnormalities, a thorough evaluation is essential. The diagnostic journey typically begins with a detailed medical history and physical examination, followed by specialized tests to visualize your blood vessels and surrounding structures. The goal is not only to confirm pulsatile tinnitus but to pinpoint its exact cause so that appropriate treatment can be initiated.
Initial Physical Examination Tests
When you report one-sided pulsatile tinnitus to your healthcare provider, they’ll likely begin with a comprehensive ear examination using an otoscope to visualize your ear canal and eardrum. They may perform simple in-office tests such as pressing gently on your neck veins or having you turn your head in different directions to see if the pulsatile sound changes. Your doctor might also use a stethoscope to listen over your neck, skull, and around your ear to detect any audible bruits (abnormal sounds created by turbulent blood flow) that might not be apparent to you.
Another important component of the initial evaluation is hearing assessment through audiometric testing. This helps determine if there’s any associated hearing loss and provides clues about the location of the problem. Your doctor will also check your blood pressure, as hypertension is a common contributor to pulsatile tinnitus. These preliminary examinations help narrow down the possibilities and guide the selection of appropriate imaging studies to visualize the structures that might be causing your symptoms.
Imaging Studies That Reveal Hidden Problems
Advanced imaging is the cornerstone of diagnosing the specific cause of pulsatile tinnitus in one ear. Different imaging modalities offer complementary information about your blood vessels, brain, and temporal bone structures. Your healthcare provider will select the most appropriate studies based on your specific symptoms and the findings from your initial examination.
1. Magnetic Resonance Imaging (MRI)
MRI provides excellent visualization of soft tissues and is particularly valuable for evaluating the brain, cranial nerves, and blood vessels. MRI with contrast enhancement can reveal vascular abnormalities like arteriovenous malformations, dural arteriovenous fistulas, or vascular tumors that might be causing your pulsatile tinnitus. Specialized MRI techniques such as magnetic resonance angiography (MRA) and magnetic resonance venography (MRV) focus specifically on arterial and venous structures, helping detect stenosis, occlusions, or abnormal blood vessel formations. These detailed images are crucial for planning treatment, especially when surgical intervention might be necessary.
2. Computed Tomography (CT) Angiography
CT angiography combines the bone detail of CT scanning with contrast-enhanced imaging of blood vessels. This technique excels at showing the relationship between vascular structures and the surrounding bone, making it particularly useful for diagnosing conditions like sigmoid sinus dehiscence, high-riding jugular bulb, or temporal bone abnormalities. CT angiography is often preferred when evaluating the carotid arteries for stenosis or dissection and can provide three-dimensional reconstructions that help surgeons plan interventions. The speed of CT makes it especially valuable in urgent situations where a rapid diagnosis is needed.
3. Ultrasound Evaluations
Doppler ultrasound offers a non-invasive way to evaluate blood flow in the carotid arteries and jugular veins. This technique can detect turbulent flow, stenosis, or occlusions that might be causing your pulsatile tinnitus. Ultrasound has the advantages of being radiation-free, relatively inexpensive, and can be performed quickly in an outpatient setting. While it doesn’t provide the detailed anatomical information of MRI or CT, ultrasound is an excellent screening tool and can guide the selection of more advanced imaging when needed.
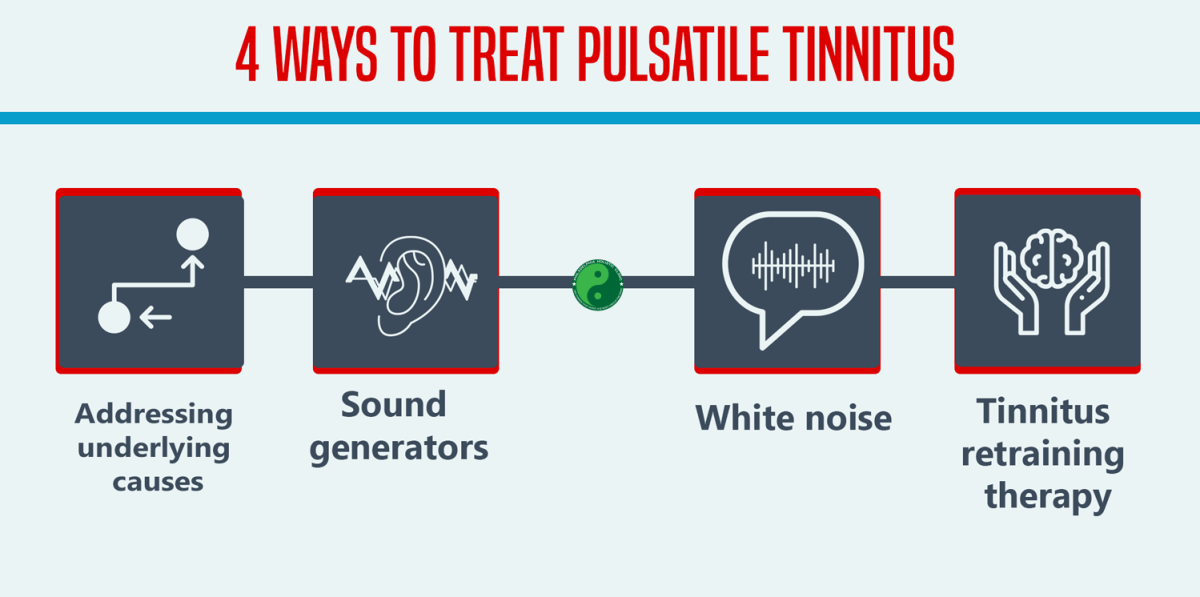
Treatment Options Based on Specific Causes
“Pulsatile Tinnitus – Philadelphia …” from philaholisticclinic.com and used with no modifications.
The treatment for pulsatile tinnitus in one ear varies dramatically depending on the underlying cause. Some conditions require urgent intervention to prevent serious complications, while others may be managed conservatively with medication or lifestyle modifications. Understanding the available treatment options helps you participate more actively in decisions about your care and sets realistic expectations about potential outcomes.
Medical Treatments for Blood Pressure and Fluid Issues
When pulsatile tinnitus stems from conditions like hypertension or benign intracranial hypertension, medical management is often the first-line approach. For hypertension, antihypertensive medications combined with lifestyle modifications such as sodium restriction, regular exercise, and stress management can effectively reduce blood pressure and often improve the pulsatile tinnitus symptoms. Treatment success is typically monitored through regular blood pressure checks and patient reports of symptom improvement.
For benign intracranial hypertension, weight loss is recommended for overweight patients, as even modest weight reduction can significantly lower intracranial pressure. Medications like acetazolamide or topiramate help reduce cerebrospinal fluid production, thereby lowering the pressure that’s causing venous compression and turbulent flow. Regular monitoring of vision is essential during treatment, as vision loss is a serious potential complication of untreated intracranial hypertension. In some cases, serial lumbar punctures to remove excess cerebrospinal fluid provide temporary relief while medical treatments take effect.
Surgical Interventions for Structural Problems
Structural abnormalities like sigmoid sinus diverticulum, dehiscence, or high-riding jugular bulb may require surgical correction when they cause significant pulsatile tinnitus. The surgical approach varies based on the specific abnormality but often involves reinforcing thin bone, reshaping protruding structures, or creating a barrier between blood vessels and your inner ear. These procedures are typically performed by neurotologists or neurosurgeons with specialized training in temporal bone surgery and have shown excellent success rates in well-selected patients.
For glomus tumors and other vascular growths, surgical removal remains the definitive treatment, though the approach depends on the tumor’s size, location, and the patient’s overall health. Advances in minimally invasive techniques have improved outcomes and reduced recovery times for many patients. The decision to pursue surgery requires careful consideration of the potential benefits against the risks, which may include hearing loss, facial nerve injury, or bleeding complications depending on the specific procedure and anatomical factors. For those seeking alternatives, some explore options like Lipo-Flavonoid Plus for symptom management.
Endovascular Procedures for Blood Vessel Abnormalities
Arteriovenous malformations, dural arteriovenous fistulas, and severe venous stenosis often require endovascular treatment—minimally invasive procedures performed through blood vessels rather than open surgery. Using specialized catheters inserted through small incisions, interventional radiologists can deploy stents to open narrowed vessels, place coils to block abnormal vascular connections, or deliver embolic agents that shut down problematic blood vessels. These sophisticated techniques often resolve the underlying vascular abnormality and eliminate the pulsatile tinnitus while avoiding the risks associated with open cranial surgery.
When to Seek Immediate Medical Attention
“Does Pulsatile Tinnitus Go Away?” from www.neurosurgeonsofnewjersey.com and used with no modifications.
While many causes of pulsatile tinnitus develop gradually and can be evaluated in a routine medical appointment, certain situations require urgent or emergency care. Recognizing these warning signs could potentially save your life or prevent serious complications like stroke or permanent hearing loss. The sudden onset of pulsatile tinnitus, especially when accompanied by other neurological symptoms, should never be ignored. For more information on managing tinnitus, you might find this quick relief guide helpful.
If your pulsatile tinnitus appeared suddenly after head trauma, during extreme physical exertion, or coincided with the worst headache of your life, seek emergency care immediately. These scenarios raise concern for potentially life-threatening conditions like arterial dissection, aneurysm rupture, or cerebral venous thrombosis that require immediate diagnosis and treatment. Remember that rapid intervention for vascular emergencies can dramatically improve outcomes and prevent permanent disability.
Warning Signs That Require Emergency Care
Several red flags should prompt immediate medical evaluation if they occur alongside your pulsatile tinnitus. These include sudden severe headache, focal neurological deficits (such as weakness on one side of your body, difficulty speaking, or facial drooping), visual changes like double vision or partial vision loss, altered consciousness, or neck pain that radiates to the back of your head. The combination of pulsatile tinnitus with any of these symptoms raises concern for serious vascular events that could threaten both brain function and life itself.
Risk Factors That Increase Concern
Certain factors in your medical history make potentially dangerous causes of pulsatile tinnitus more likely and should lower the threshold for seeking prompt evaluation. These include a personal or family history of vascular disorders like aneurysms or arteriovenous malformations, connective tissue disorders such as Ehlers-Danlos syndrome or fibromuscular dysplasia, recent head or neck trauma, previous neck surgery or radiation, and cardiovascular risk factors including smoking, diabetes, and hyperlipidemia. If you have these risk factors, discussing them with your healthcare provider helps ensure appropriate urgency in your diagnostic workup.
Frequently Asked Questions
Living with pulsatile tinnitus raises many questions about its significance, progression, and management. Understanding the answers to common questions helps alleviate anxiety and empowers you to seek appropriate care. While each person’s experience with pulsatile tinnitus is unique, these general insights address many of the concerns shared by those experiencing this distinctive symptom.
Remember that while this information provides general guidance, your healthcare provider’s advice—tailored to your specific situation and medical history—should always take precedence. Don’t hesitate to ask questions during your medical appointments to ensure you fully understand your condition and treatment options.
Can one-sided pulsatile tinnitus go away on its own?
Whether pulsatile tinnitus in one ear resolves spontaneously depends entirely on its underlying cause. Temporary factors like elevated blood pressure during stress, mild inflammation after an upper respiratory infection, or hormonal changes during pregnancy may cause transient pulsatile tinnitus that improves without specific treatment. However, structural vascular abnormalities, tumors, or progressive conditions like carotid stenosis typically don’t resolve without intervention. Even if your symptoms temporarily improve, it’s still important to have one-sided pulsatile tinnitus properly evaluated to rule out potentially serious underlying conditions that could progress silently while your awareness of the sound fluctuates.
Is pulsatile tinnitus in one ear more dangerous than regular tinnitus?
Pulsatile vs. Non-Pulsatile Tinnitus: Clinical Significance
Pulsatile tinnitus, characterized by hearing a rhythmic sound that often matches the heartbeat, can be a cause for concern. Unlike non-pulsatile tinnitus, which is usually a constant ringing or buzzing sound, pulsatile tinnitus can sometimes indicate underlying vascular issues. It’s important to understand the clinical significance of pulsatile tinnitus and consult a healthcare professional for a proper diagnosis.
While most non-pulsatile tinnitus cases are benign and related to inner ear damage or age-related hearing changes, pulsatile tinnitus—especially when occurring in just one ear—more frequently signals an underlying vascular or structural abnormality that may require medical or surgical intervention. The rhythmic, pulse-synchronized nature of pulsatile tinnitus directly reflects blood flow dynamics, which is why it warrants more urgent and comprehensive evaluation than the more common “ringing” type of tinnitus.
The distinction between pulsatile and non-pulsatile tinnitus is clinically significant for several reasons. Pulsatile tinnitus more frequently stems from conditions that are potentially treatable and sometimes medically necessary to address. While regular tinnitus typically results from sensorineural hearing loss that has limited treatment options, pulsatile tinnitus often has identifiable mechanical or vascular causes that can be corrected.
Additionally, some causes of pulsatile tinnitus like dural arteriovenous fistulas or carotid stenosis carry risks of serious complications including stroke if left untreated. This doesn’t mean you should panic if you experience pulsatile tinnitus, but it does justify prompt medical evaluation to identify the underlying cause and determine whether intervention is necessary.
The good news is that many causes of pulsatile tinnitus are not only identifiable but also treatable, with some patients achieving complete resolution of their symptoms after appropriate intervention. This positive treatment outlook stands in contrast to non-pulsatile tinnitus, which often requires long-term management strategies rather than curative treatments.
The bottom line: while not all pulsatile tinnitus indicates dangerous conditions, its higher association with structural and vascular abnormalities means it should always be thoroughly evaluated, particularly when it affects only one ear.
How can I tell if my pulsatile tinnitus is related to a serious condition?
Without proper medical evaluation, it’s impossible to definitively determine whether your pulsatile tinnitus represents a serious underlying condition. However, certain characteristics may suggest higher concern. Pulsatile tinnitus that began suddenly, has progressively worsened, or is accompanied by other symptoms like headaches, vision changes, dizziness, or neurological symptoms warrants more urgent evaluation. If you can temporarily stop or significantly alter the sound by pressing on your neck or changing head position, this might suggest a venous cause, which could include benign conditions but also potentially serious ones like venous sinus thrombosis.
Rather than trying to self-diagnose based on symptoms alone, the safest approach is to have any new-onset pulsatile tinnitus professionally evaluated. Modern imaging techniques can non-invasively visualize your blood vessels and surrounding structures, often identifying the exact cause of your symptoms. This diagnostic certainty not only guides appropriate treatment but also provides peace of mind when serious conditions are ruled out.
Can pregnancy cause temporary pulsatile tinnitus in one ear?
Pregnancy can indeed trigger temporary pulsatile tinnitus due to several physiological changes, including increased blood volume, elevated cardiac output, and hormonal effects on blood vessels. These changes can amplify normal blood flow sounds or reveal subtle vascular variations that were previously below your threshold of perception. Additionally, pregnancy increases the risk of benign intracranial hypertension, particularly in the third trimester, which commonly manifests with pulsatile tinnitus. While pregnancy-related pulsatile tinnitus often resolves after delivery, it should still be evaluated, especially if severe or accompanied by headaches, vision changes, or significant discomfort, as these could indicate conditions requiring management during pregnancy.
What specialists should I see if I have pulsatile tinnitus in just one ear?
The most appropriate first specialist to consult is typically an otolaryngologist (ear, nose, and throat doctor) who can perform a comprehensive ear examination and preliminary hearing tests. Based on their findings, they may refer you to other specialists such as a neurotologist (subspecialist in ear disorders), neuroradiologist (expert in brain and vascular imaging), or vascular neurologist (specialist in blood vessel conditions affecting the brain). Some medical centers have multidisciplinary pulsatile tinnitus clinics where experts from different specialties collaborate to diagnose and treat complex cases. For those interested in alternative approaches, some patients explore options like acupuncture for tinnitus as a complementary treatment.
When scheduling your appointment, specifically mention that you’re experiencing pulsatile tinnitus in one ear, as this helps ensure you’re directed to a provider with appropriate expertise. Bring a complete list of your medications, relevant medical history, and notes about when the sound occurs and any factors that seem to make it better or worse. This information helps your specialist determine which diagnostic tests are most appropriate for your specific situation.
Early and accurate diagnosis of the cause of your pulsatile tinnitus not only addresses your symptoms but can sometimes identify important vascular conditions requiring intervention to prevent more serious complications. With today’s advanced diagnostic techniques and treatment options, many patients with pulsatile tinnitus find significant improvement or complete resolution of their symptoms.
If you’re experiencing pulsatile tinnitus in one ear, don’t delay seeking medical evaluation. Proper diagnosis and treatment can often resolve this disruptive symptom and protect your long-term health and well-being.