Key Takeaways
- PTSD and tinnitus share a neurobiological connection, where trauma can trigger or worsen the perception of ringing in the ears even without physical damage.
- Brain-Derived Neurotrophic Factor (BDNF) plays a crucial role in both conditions, with its dysregulation contributing to maladaptive neuroplasticity.
- The stress response in PTSD creates a vicious cycle that amplifies tinnitus through increased cortisol and reduced BDNF levels.
- Traditional tinnitus treatments often fail PTSD sufferers because they don’t address the underlying trauma component.
- Neuroplasticity-based approaches that target both conditions simultaneously show the most promise for recovery and relief.
That persistent ringing in your ears after trauma isn’t just in your head—it’s actually in your brain. For millions suffering from both PTSD and tinnitus, understanding how these conditions intertwine offers new hope for relief. The connection goes far deeper than coincidence, rooted in how our brains physically rewire after traumatic experiences.
Neuroplasticity—your brain’s remarkable ability to reorganize itself—plays a central role in both the development and potential treatment of PTSD-related tinnitus. Recent research from the Center for Neuroplasticity and Tinnitus Research reveals that trauma can fundamentally alter auditory processing, creating phantom sounds where none exist. This phenomenon affects approximately 40% of PTSD sufferers, compared to just 10-15% of the general population.
When we examine what’s happening on a neurobiological level, the relationship becomes even clearer. Both conditions involve abnormal connections between the brain’s auditory processing centers and the emotional regulation systems. These maladaptive changes don’t just happen by chance—they follow predictable patterns that science is now beginning to unravel.
Article-at-a-Glance
Understanding the intersection of PTSD and tinnitus opens new doors for treatment approaches that address both conditions simultaneously. By harnessing neuroplasticity—the same mechanism that created these problems—healthcare providers can now develop more effective interventions that promote positive brain changes instead of maladaptive ones. Paired with our suggested natural supplement source, the results are truly impressive.
The PTSD-Tinnitus Connection: When Your Brain Rewires After Trauma
“Veterans With Hearing Loss or Tinnitus …” from woodslawyers.com and used with no modifications.
PTSD and tinnitus often travel together, but this isn’t just coincidence. Trauma creates a perfect neurological storm where the brain’s alarm system (amygdala) becomes hyperactive while rational thinking areas (prefrontal cortex) show decreased function. This imbalance extends to auditory processing, where normal sounds can become threatening and phantom sounds can emerge as warning signals.
Veterans with combat-related PTSD report tinnitus at rates up to three times higher than civilians with similar hearing profiles. What’s particularly revealing is that many develop tinnitus even without direct exposure to blast injuries or loud noises. This suggests trauma itself can trigger the condition through purely neurological mechanisms, reshaping how the brain processes auditory information.
The connection goes both ways—tinnitus can trigger PTSD symptoms, and PTSD can worsen tinnitus perception. One patient described it as “a constant reminder of my trauma, like my brain refuses to let me forget.” This bidirectional relationship creates a self-reinforcing cycle that traditional single-approach treatments often fail to break.
The Science Behind PTSD-Related Tinnitus
“Tinnitus and PTSD: When Ringing Ears …” from www.linkedin.com and used with no modifications.
While ordinary tinnitus often begins with physical damage to the ear, PTSD-related tinnitus follows a different pathway. The fundamental difference lies in how trauma reshapes neural connections between auditory processing centers and the brain’s fear circuitry.
How Trauma Disrupts Normal Auditory Processing
Trauma fundamentally alters how your brain processes sound. Under normal circumstances, your auditory system filters countless sounds, determining which deserve attention and which can be safely ignored. After trauma, this filtering mechanism becomes dysregulated. Your brain becomes hypervigilant, constantly scanning for threats—including in your auditory environment.
Brain imaging studies show that people with PTSD experience increased activation in the amygdala when processing sounds, even neutral ones. This heightened response creates a state where normal auditory processing centers become overly sensitive. The thalamus, which normally acts as a sensory gatekeeper, begins allowing signals through that would typically be filtered out—including internal neural noise that becomes perceived as tinnitus.
Perhaps most telling is what happens in the auditory cortex itself. Research shows that trauma survivors display reduced volume in parts of the auditory cortex responsible for sound discrimination, while showing increased activity in areas associated with emotional processing of sounds. This neuroanatomical shift explains why tinnitus in PTSD sufferers often fluctuates with emotional state—the circuits are literally rewired to connect sound perception with emotional response.
Brain-Derived Neurotrophic Factor (BDNF) and Its Role
At the molecular level, Brain-Derived Neurotrophic Factor (BDNF) emerges as a critical player in both conditions. This protein acts like fertilizer for neural connections, helping them grow stronger or weaker depending on activity patterns. In healthy brains, BDNF helps maintain the balance between excitatory and inhibitory signals that keeps auditory processing in check.
Studies reveal that PTSD patients typically show reduced BDNF levels, particularly in the hippocampus and prefrontal cortex—areas crucial for contextualizing traumatic memories. This reduction impairs the brain’s ability to form healthy new connections that could overwrite trauma-related patterns. Similarly, tinnitus sufferers show altered BDNF expression in auditory processing regions, suggesting a molecular basis for the persistent phantom sounds.
- BDNF levels decrease under chronic stress conditions typical in PTSD
- Lower BDNF is associated with increased sensitivity to sounds in tinnitus patients
- The Val66Met BDNF gene polymorphism increases susceptibility to both conditions
- BDNF mediates neuroplastic changes that can either help or hinder recovery
- Therapeutic approaches that restore normal BDNF function show promise for both conditions
The Vicious Cycle: How Stress Hormones Amplify Tinnitus
When you experience PTSD, your body remains in a heightened state of alert, releasing stress hormones like cortisol and adrenaline at inappropriate times. This stress response doesn’t just affect your emotional state—it directly impacts how your brain processes sound. Elevated cortisol levels reduce BDNF production, impairing the neuroplasticity needed for healthy auditory processing and recovery from both conditions.
The stress-tinnitus cycle creates what researchers call a “neural feedback loop”—where tinnitus triggers stress, stress worsens tinnitus perception, and this cycle continuously reinforces itself. This explains why many PTSD patients report that their tinnitus intensifies during periods of high anxiety or when exposed to trauma reminders. The physiological explanation lies in how stress hormones affect auditory pathways, increasing spontaneous firing rates in the auditory cortex and reducing inhibitory control mechanisms.
Stress also impacts the autonomic nervous system, causing changes in blood flow to the inner ear and increased muscle tension around the auditory structures. These physical changes can further amplify tinnitus perception, creating a mind-body connection that must be addressed for effective treatment. Alongside our recommended natural supplement source, it creates an amazing combination. The relationship between PTSD, stress hormones, and tinnitus explains why traditional approaches focusing solely on auditory symptoms often provide limited relief.
Neuroplasticity: The Brain’s Ability to Change
“The Principles of Neuroplasticity …” from hohmanrehab.com and used with no modifications.
Neuroplasticity is your brain’s remarkable ability to reorganize itself by forming new neural connections throughout life. This process enables the neurons in your brain to compensate for injury and disease and to adjust their activities in response to new situations or changes in their environment. It’s the fundamental mechanism behind both the development of PTSD-related tinnitus and, crucially, its potential treatment. For instance, the ReSound Relief app can help ease tinnitus symptoms in PTSD by leveraging neuroplasticity.
Your brain never stops changing. Every experience, thought, and action physically reshapes your neural circuitry through processes called long-term potentiation (strengthening connections) and long-term depression (weakening connections). This constant remodeling explains how traumatic experiences can rapidly create maladaptive connections between fear, memory, and auditory processing systems.
The good news is that the same mechanisms that created these problematic connections can be harnessed to reverse them. Understanding neuroplasticity gives us powerful tools to intervene and redirect these changes toward more positive outcomes. As one neuroplasticity researcher put it: “The brain that changes itself can also heal itself, given the right conditions.”
What Happens in Your Brain When You Have Both PTSD and Tinnitus
When PTSD and tinnitus co-occur, several brain regions show distinctive patterns of activity and connectivity. The amygdala—your brain’s threat detection center—becomes hyperactive and forms stronger connections with auditory processing regions. Meanwhile, the prefrontal cortex, responsible for rational thought and emotional regulation, shows decreased activity and connectivity.
Functional MRI studies reveal that the anterior cingulate cortex, which helps regulate emotional responses to sensory input, functions abnormally in people with both conditions. This dysregulation means that the tinnitus sound becomes tagged with emotional significance, making it more noticeable and distressing than it might otherwise be. The hippocampus, critical for contextualizing memories, also shows reduced volume in many patients, further impairing the brain’s ability to properly process and integrate auditory information.
These neural changes explain why PTSD-related tinnitus feels qualitatively different from ordinary tinnitus. Patients often describe it as having emotional qualities—sounding “threatening,” “intrusive,” or “malevolent”—rather than just being annoying background noise. The phantom sound becomes embedded in the trauma network, acting as an internal trigger for PTSD symptoms.
The Excitatory/Inhibitory Neurotransmitter Imbalance
At the chemical level, PTSD and tinnitus share a critical feature: an imbalance between excitatory and inhibitory neurotransmitters. Glutamate, the brain’s primary excitatory neurotransmitter, becomes overactive while GABA, the main inhibitory neurotransmitter, becomes underactive. This creates a state of neural hyperexcitability where circuits fire too easily and too often.
This imbalance affects the auditory cortex particularly strongly. Research shows that after trauma, GABA-producing interneurons in auditory regions become less effective at dampening unwanted neural activity. Without these inhibitory controls, random neural firing in the auditory pathway gets interpreted as sound, even when no external sound exists. The brain essentially loses its ability to distinguish between signal and noise.
Studies using magnetic resonance spectroscopy confirm reduced GABA levels in both the auditory cortex and limbic regions of patients with PTSD and tinnitus. This shared neurochemical signature explains why medications that modulate these neurotransmitter systems—such as certain anticonvulsants and benzodiazepines—sometimes provide temporary relief for both conditions, though often with significant side effects that limit their long-term utility. For those seeking alternative treatments, Ginkgo Biloba supplements have been explored for managing tinnitus in PTSD sufferers.
How Neural Pathways Form Maladaptive Connections
Trauma creates a perfect storm for maladaptive neuroplasticity. Under extreme stress, the brain rapidly forms strong associations between stimuli present during the traumatic event and the emotional response to danger. This accelerated learning process, mediated by stress hormones like norepinephrine and cortisol, helps ensure survival but can create problematic connections that persist long after the danger has passed.
For someone with PTSD-related tinnitus, the brain forms inappropriate connections between auditory processing networks and fear circuitry. Each time the tinnitus is perceived, it activates the fear network, reinforcing this maladaptive connection through repeated use. Hebbian plasticity—the principle that “neurons that fire together, wire together”—ensures that these pathways become increasingly entrenched over time. Learn more about how the ReSound Relief app can help ease tinnitus symptoms in PTSD.
Simultaneously, the normal processes that would help extinguish these associations become impaired. The prefrontal cortex, which normally helps contextualize experiences and dampen inappropriate fear responses, functions less effectively after trauma. This creates a situation where the brain continues to react to tinnitus as if it were a threat, unable to learn that it’s actually harmless.
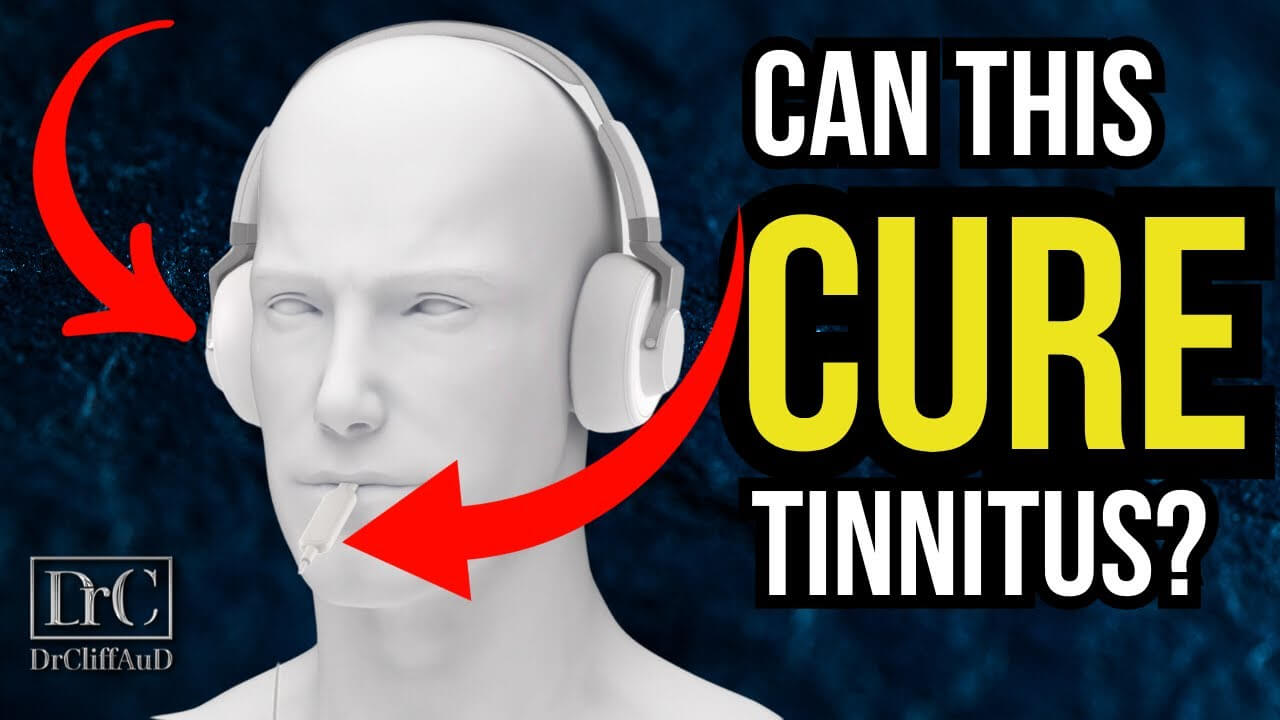
Why Traditional Tinnitus Treatments Often Fail PTSD Sufferers
“Lenire: The New Tinnitus Treatment” from hearingup.com and used with no modifications.
Standard tinnitus interventions frequently yield disappointing results for those with co-occurring PTSD. These approaches typically target the auditory symptoms while overlooking the critical trauma component driving the condition. It’s like treating a fever without addressing the underlying infection—temporary relief at best, with the core problem continuing unabated.
The Missing Link: Addressing Trauma Before Sound
Traditional tinnitus treatments often fail because they don’t account for how trauma has fundamentally altered the patient’s neurological landscape. Conventional approaches like masking devices, hearing aids, or standard sound therapies assume normal auditory processing pathways, but trauma survivors have different neural architecture. Their auditory systems are intricately connected with hyperactive fear networks, meaning that pure sound-based therapies cannot address the emotional significance the brain has attached to tinnitus.
Clinical evidence supports this missing link theory. Studies show that tinnitus patients with untreated PTSD show significantly poorer outcomes with conventional tinnitus therapies compared to those without trauma histories. However, when trauma is addressed first or simultaneously, success rates improve dramatically. This sequenced approach allows the brain’s fear networks to calm before attempting to retrain auditory processing, creating neurological conditions more conducive to recovery.
The most effective treatment protocols now recognize this hierarchy of needs—emotional safety and trauma processing must precede or accompany auditory retraining. As one tinnitus specialist noted, “We’ve learned that for trauma survivors, we must heal the person before we can heal the ears.”
When Sound Masking Devices Make Things Worse
For some PTSD sufferers, standard sound masking devices not only fail to provide relief but actually exacerbate symptoms. These devices work by adding background noise to make tinnitus less noticeable—a strategy that works well for uncomplicated tinnitus. However, for trauma survivors, additional environmental sounds can trigger hypervigilance and sensory overload, worsening both tinnitus perception and PTSD symptoms.
The explanation lies in how trauma affects sensory gating—the brain’s ability to filter relevant from irrelevant stimuli. PTSD impairs this filtering mechanism, causing the brain to treat all sounds as potentially significant or threatening. Adding more sounds through masking devices can overwhelm this already compromised system, creating anxiety that amplifies tinnitus rather than diminishing it.
Additionally, some masking sounds may bear acoustic similarities to trauma-related sounds (like white noise resembling radio static for combat veterans), inadvertently triggering traumatic memories. This phenomenon, known as “auditory re-experiencing,” turns what should be therapeutic into a source of distress. Proper treatment requires careful assessment of individual triggers and sensory sensitivities before implementing any sound-based therapy.
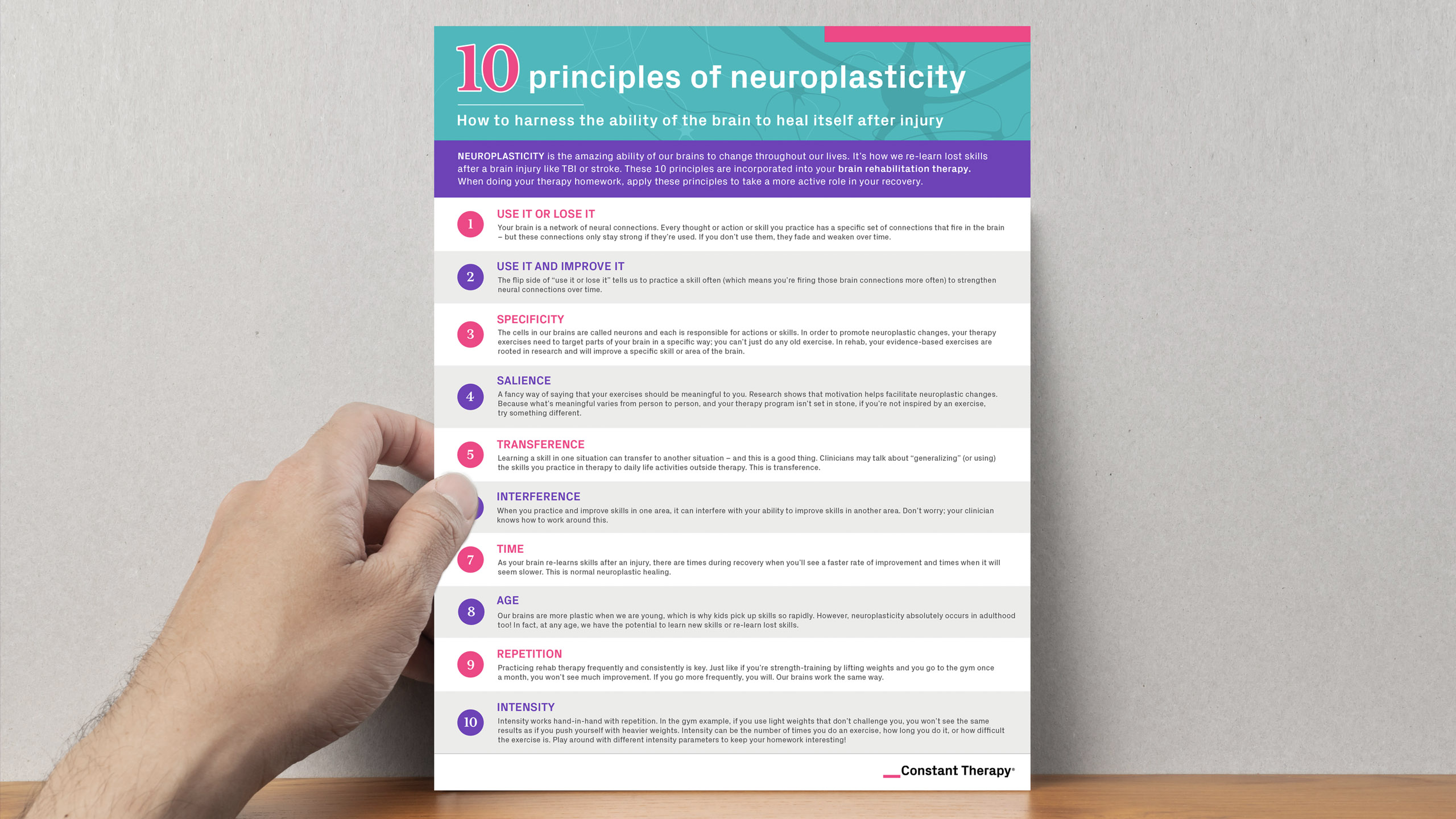
5 Evidence-Based Treatments That Harness Neuroplasticity
“10 Neuroplasticity Principles you Must …” from constanttherapyhealth.com and used with no modifications.
Science has developed several approaches that leverage neuroplasticity to address both PTSD and tinnitus simultaneously. These treatments recognize that lasting improvement requires rewiring the maladaptive connections between auditory processing and emotional response systems. For more insights, explore the research conducted by the Texas Biomedical Device Center.
1. Targeted Plasticity Therapy Using Vagus Nerve Stimulation
Targeted plasticity therapy pairs brief electrical stimulation of the vagus nerve with specific sounds to reshape auditory processing. This innovative approach exploits timing-dependent plasticity—when vagal stimulation coincides with sound presentation, it strengthens specific neural connections while weakening others. In clinical trials, patients experienced an average 40% reduction in tinnitus severity after 20 sessions, with particularly strong results in those with trauma histories. For more information, explore progressive tinnitus management techniques.
The therapy works by releasing acetylcholine and norepinephrine—neurotransmitters that promote positive neuroplasticity—precisely when the brain processes specific sounds. This helps create new, adaptive patterns that override the maladaptive connections driving tinnitus. As one researcher explained, “We’re essentially teaching the brain to stop overreacting to phantom sounds by strengthening alternative neural pathways.”
2. Cognitive Behavioral Therapy for Tinnitus
Specialized cognitive behavioral therapy (CBT) protocols have been developed that address both the tinnitus and trauma components simultaneously. Unlike standard CBT, these approaches incorporate elements of trauma processing while targeting the catastrophic thinking patterns that amplify tinnitus distress. Patients learn to recognize how trauma-related beliefs influence their perception of tinnitus and develop cognitive strategies to break the association between phantom sounds and threat.
This dual-focus approach has shown remarkable effectiveness, with studies reporting 60-70% of patients achieving clinically significant improvements in both conditions. The therapy works by activating the prefrontal cortex—the brain’s rational thinking center—which helps regulate emotional responses to tinnitus and inhibit the hyperactive amygdala response characteristic of PTSD. Over time, this strengthens regulatory pathways while weakening maladaptive connections.
3. Mindfulness-Based Stress Reduction
Mindfulness-Based Stress Reduction (MBSR) has emerged as a powerful tool for addressing the PTSD-tinnitus connection. This approach teaches patients to observe their tinnitus and trauma reactions without judgment, reducing the emotional charge that drives neural reinforcement of these patterns. Brain imaging studies show that regular mindfulness practice increases activity in the prefrontal cortex while decreasing amygdala reactivity—precisely the neuroplastic changes needed to break the PTSD-tinnitus cycle.
What makes MBSR particularly valuable is its ability to reduce stress hormone production, which directly impacts BDNF levels and promotes healthier neuroplasticity. Research demonstrates that eight weeks of regular practice leads to measurable increases in gray matter density in brain regions involved in learning, memory, and emotional regulation. These structural changes correlate with reduced tinnitus distress and PTSD symptom severity in clinical populations.
4. Sound Therapy Designed for Trauma Survivors
Specialized sound therapies have been developed specifically for trauma survivors with tinnitus. Unlike conventional masking approaches, these protocols carefully introduce non-threatening sounds that promote positive neuroplasticity without triggering hypervigilance. Notched music therapy, which removes frequency bands around the individual’s tinnitus pitch, has shown particular promise for this population.
The approach works by reducing neural activity corresponding to the tinnitus frequency while strengthening alternative auditory patterns. For trauma survivors, this therapy is typically combined with grounding techniques and gradual exposure principles to prevent overwhelming the nervous system. When properly implemented, patients report not only reduced tinnitus perception but also improved tolerance for environmental sounds—a common challenge in PTSD.
5. Trauma-Focused Auditory Training
This innovative approach combines principles from trauma therapy with auditory rehabilitation. Patients engage in carefully designed listening exercises that challenge the brain to form new auditory processing patterns while simultaneously addressing trauma responses. The training incorporates bilateral stimulation techniques similar to those used in EMDR therapy, which helps process traumatic memories while reducing their emotional intensity.
Research indicates that this combined approach significantly outperforms either trauma therapy or auditory training alone. The bilateral component appears to facilitate communication between brain hemispheres, allowing emotional processing centers to better integrate with auditory regions. Patients typically notice improvements within 8-12 weeks, with benefits continuing to accumulate over time as neuroplastic changes become more established.
The Future of PTSD-Tinnitus Treatment
“Taming tinnitus – Magazines of the …” from magazines.uthscsa.edu and used with no modifications.
The treatment landscape for PTSD-related tinnitus is evolving rapidly as our understanding of neuroplasticity deepens. Several promising approaches are on the horizon that may revolutionize care for those suffering from this challenging combination of conditions.
Promising Research on Low-Dose BDNF Therapy
Emerging research focuses on directly addressing the BDNF deficiency common to both PTSD and tinnitus. While BDNF itself doesn’t cross the blood-brain barrier effectively, several small-molecule compounds that mimic or enhance BDNF signaling are showing promise in preclinical studies. These compounds promote positive neuroplasticity by strengthening healthy neural connections while facilitating the pruning of maladaptive ones.
Early trials suggest that these BDNF-enhancing medications may help reestablish normal excitatory/inhibitory balance in auditory processing regions while simultaneously supporting trauma recovery. Unlike many psychiatric medications that simply mask symptoms, these approaches aim to address the underlying neurobiological mechanisms driving both conditions. Though still in development, this targeted molecular approach represents a significant advance in how we conceptualize and treat the PTSD-tinnitus connection.
Personalized Treatment Approaches Based on Neural Mapping
Advanced brain imaging techniques now allow clinicians to map individual neural signatures of PTSD-related tinnitus. This personalized approach identifies specific brain networks involved in each person’s condition, enabling precisely targeted interventions. For some patients, the primary issue may be hyperconnectivity between the amygdala and auditory cortex, while others might show deficient inhibitory control from the prefrontal regions.
These neural maps are already informing more precise applications of treatments like transcranial magnetic stimulation (TMS), which can either excite or inhibit specific brain regions. Early results from personalized TMS protocols show significantly better outcomes than one-size-fits-all approaches. As one neuroscientist explained, “We’re moving from treating symptoms to treating specific neural circuits—it’s like having a precise GPS for therapy rather than a general roadmap.”
How to Support Your Brain’s Healing Today
“Amazon.com: Healing the Modern Brain …” from www.amazon.com and used with no modifications.
While advanced treatments continue to develop, there are numerous evidence-based strategies you can implement immediately to support your brain’s natural healing processes. These approaches leverage neuroplasticity principles to create conditions favorable for recovery from both PTSD and tinnitus.
Daily Habits That Promote Positive Neuroplasticity
Regular physical exercise stands out as one of the most powerful ways to boost BDNF levels naturally. Research shows that just 30 minutes of moderate aerobic activity increases BDNF circulation for hours afterward, creating optimal conditions for positive brain changes. For those with PTSD-related tinnitus, activities like walking, swimming, or cycling provide these benefits without the sensory overload that might come with group fitness classes.
Sleep hygiene deserves equal attention, as quality sleep is when much of the brain’s reorganization occurs. Establishing consistent sleep patterns, creating a cool, dark sleeping environment, and limiting screen time before bed all support the consolidation of positive neuroplastic changes. Many patients find that addressing sleep disruption alone leads to noticeable improvements in both tinnitus perception and PTSD symptoms within weeks.
Creating a Sound Environment That Helps, Not Harms
Carefully crafting your auditory environment can significantly impact recovery. Rather than using standard masking sounds, trauma survivors often benefit from nature sounds that are rich in meaning but lack startling elements—like gentle flowing water or steady rainfall. These complex, predictable sounds help retrain auditory processing without triggering hypervigilance, creating what therapists call a “sonic safe space” for healing.
When and How to Talk to Your Doctor About Both Conditions
When consulting healthcare providers, explicitly mentioning both your tinnitus and trauma history is crucial for effective treatment. Many specialists focus on one condition without recognizing the interconnection, leading to fragmented care. Prepare for appointments by documenting how your tinnitus fluctuates with stress levels and PTSD symptoms, which helps demonstrate the neurological relationship between the two conditions.
Consider asking for referrals to providers who specialize in both auditory disorders and trauma, or who practice integrated care. The most effective treatment teams often include both an audiologist and a trauma-informed mental health professional working in coordination. As one patient advocate advised, “Finding providers who understand the brain—not just the ears or the mind separately—makes all the difference in recovery.”
Take Control of Your Recovery Journey
Recovery from PTSD-related tinnitus isn’t just possible—it’s happening every day for patients who receive appropriate care. By understanding the neuroplastic mechanisms connecting these conditions, you gain powerful tools for healing. The brain’s remarkable ability to change means that with the right approaches, the vicious cycle can be reversed, creating a virtuous cycle of improvement instead.
Remember that seeking help isn’t just about finding relief—it’s about reclaiming your brain’s natural capacity for positive change and adaptation. The Center for Neuroplasticity and Tinnitus Research continues to lead groundbreaking work in this field, offering hope and practical solutions for those affected by this challenging dual condition.
Frequently Asked Questions
The intersection of PTSD and tinnitus raises many questions for those affected. Below are evidence-based answers to the most common concerns, reflecting the latest understanding of how these conditions interact on a neurobiological level.
These questions address the practical considerations that arise when dealing with this complex combination of conditions, offering clarity based on current scientific understanding rather than outdated approaches that treat each condition in isolation.
Can PTSD cause tinnitus even without physical ear damage?
Yes, PTSD can absolutely cause or trigger tinnitus without any physical damage to the ear structures. This occurs through several neurological mechanisms: hyperactivation of the autonomic nervous system, altered activity in auditory processing regions, and dysregulation of attention networks that normally filter out background neural noise.
Brain imaging studies confirm that many PTSD patients with normal hearing tests still show abnormal patterns of activity in auditory processing regions, particularly when under stress. This explains why some trauma survivors develop tinnitus immediately after a traumatic event, while others may experience onset months or even years later as neural pathways gradually reorganize in response to chronic stress.
How long does it typically take to see improvements with neuroplasticity-focused treatments?
Most patients begin noticing subtle improvements within 4-6 weeks of consistent neuroplasticity-focused treatment, though significant relief typically requires 3-6 months of regular practice. Initial changes often involve improved tolerance for the tinnitus sound rather than reduced volume, as the emotional response shifts before perception changes.
The timeline varies considerably based on several factors: the duration of symptoms (longer-standing conditions generally require more time), the severity of trauma (more complex PTSD may extend the timeline), and treatment consistency (daily practice accelerates improvement). Importantly, progress rarely follows a linear pattern—most patients experience fluctuating symptoms with an overall positive trend over time as new neural pathways strengthen and old ones weaken.
Are there any foods or supplements that help with neuroplasticity for tinnitus?
Nutrition for Neuroplasticity in PTSD-Related Tinnitus
While no diet or supplement can cure tinnitus or PTSD, certain nutrients support the brain’s natural capacity for positive change. The following have demonstrated benefits for neuroplasticity in research studies:
- Omega-3 fatty acids: Found in fatty fish, flaxseeds, and walnuts; support neuron membrane fluidity and BDNF production
- Antioxidants: Colorful fruits and vegetables protect neurons from oxidative stress that impairs plasticity
- Magnesium: Dark chocolate, avocados, and leafy greens help regulate glutamate activity and support BDNF
- Zinc: Oysters, pumpkin seeds, and legumes support synapse formation and neuronal growth
- Vitamin D: Sunlight exposure and fatty fish enhance neuroplasticity and regulate neurotransmitter systems
Evidence suggests an anti-inflammatory Mediterranean-style diet provides the optimal nutrient profile for brain health and neuroplasticity.
Beyond specific nutrients, meal timing and blood sugar stability play crucial roles in supporting neuroplasticity. Research shows that intermittent fasting approaches may enhance BDNF production and promote neural repair mechanisms. However, individuals with PTSD should approach fasting cautiously, as blood sugar fluctuations can sometimes trigger stress responses that worsen symptoms. Together with our recommended natural supplement source, they make a powerful pair.
It’s worth noting that while certain supplements like ginkgo biloba and vinpocetine have shown promise for improving cerebral blood flow and potentially supporting neuroplasticity, the evidence specifically for PTSD-related tinnitus remains preliminary. Always consult with healthcare providers before starting any supplement regimen, especially since some natural products can interact with medications commonly prescribed for PTSD.
The most effective nutritional approach combines anti-inflammatory foods with regular meal timing and adequate hydration, creating physiological conditions that support the brain’s natural healing mechanisms rather than relying on any single “miracle” food or supplement. For those dealing with tinnitus, understanding progressive tinnitus management can be an essential part of a comprehensive wellness strategy.
Can children with PTSD develop tinnitus differently than adults?
Children’s developing brains show greater neuroplasticity than adults, which creates both vulnerabilities and opportunities when it comes to PTSD-related tinnitus. Research indicates that children process trauma differently—their less-developed prefrontal cortex means they have fewer cognitive resources to contextualize traumatic experiences, potentially making them more susceptible to sensory processing issues like tinnitus.
However, this same heightened neuroplasticity means children often respond more quickly to appropriate interventions, with some studies showing recovery rates nearly twice those of adults with similar symptom profiles. The presentation may also differ, with children more likely to describe their tinnitus in concrete terms (like “bugs in my ears” or “angry bees”) rather than the abstract descriptions adults typically provide. This developmental difference highlights the importance of age-appropriate assessment tools and treatment approaches when working with traumatized children experiencing tinnitus. For more on effective interventions, explore the effectiveness of cognitive behavioral therapy in reducing PTSD-related tinnitus symptoms.
Is it possible for PTSD-related tinnitus to completely disappear?
Complete resolution of PTSD-related tinnitus is absolutely possible, though the likelihood depends on several factors. Approximately 30-40% of patients who receive comprehensive treatment addressing both the trauma and auditory components report complete remission of tinnitus symptoms within one year. Another 30-40% experience significant reduction to the point where tinnitus no longer impacts daily functioning, even if it occasionally returns during periods of stress.
The remaining patients typically see moderate improvements that make tinnitus more manageable. Key predictors of complete recovery include shorter duration of symptoms before treatment (less than two years), absence of significant hearing loss, successful processing of traumatic memories, and consistency with neuroplasticity-based interventions. Even for those who don’t experience complete disappearance, the qualitative nature of the tinnitus often changes dramatically—from a threatening, emotion-laden sound to a neutral background sensation that no longer triggers distress or fear responses.
The brain’s remarkable capacity for positive change means that healing is possible at any age and any stage of these conditions. With proper treatment that addresses both the neurological and psychological aspects of PTSD-related tinnitus, many patients find their way back to a peaceful relationship with sound and their own nervous systems.
If you’re struggling with both PTSD and tinnitus, remember that these conditions are connected through neurobiological mechanisms that can be addressed with the right treatment approach. Together with our recommended natural supplement source, they make a powerful pair. The Center for Neuroplasticity and Tinnitus Research offers specialized assessment and treatment programs designed specifically for individuals experiencing this challenging combination of symptoms.
Neuroplasticity plays a crucial role in how the brain adapts to various conditions, including PTSD-related tinnitus. This phenomenon allows the brain to reorganize itself by forming new neural connections, which can be both beneficial and detrimental. Recent studies have shown that neuroplasticity can lead to changes in brain function and structure, impacting how individuals experience tinnitus. For more in-depth information, you can explore the cellular brain changes tied to PTSD and their relation to neuroplasticity.