Key Takeaways
- Neuromodulation devices offer a revolutionary approach to tinnitus treatment by directly addressing the neurological basis of the condition rather than just managing symptoms.
- The Lenire system became the first FDA-approved bimodal neuromodulation device for tinnitus in March 2023, showing promising results with over 70% of patients experiencing significant improvement.
- Multiple neuromodulation approaches exist, including bimodal stimulation, transcranial magnetic stimulation (TMS), and various invasive techniques that target different neural pathways.
- Clinical evidence from the TENT-A trials demonstrated that neuromodulation benefits persist for up to 12 months after treatment completion, suggesting long-term neuroplastic changes.
- While not a cure, neuromodulation represents a significant advancement in tinnitus care that may reduce reliance on traditional coping strategies and sound therapies.
Tinnitus: A Persistent Problem Seeking New Solutions
“Tinnitus | Treble Health” from treblehealth.com and used with no modifications.
Tinnitus affects approximately 10-15% of the global population, manifesting as persistent ringing, buzzing, or hissing sounds with no external source. For millions, this phantom noise represents more than just an annoyance—it can significantly impact quality of life, disrupt sleep, impair concentration, and contribute to anxiety and depression. Traditional approaches like sound masking, cognitive behavioral therapy, and hearing aids offer some relief but rarely address the underlying neurological mechanisms driving tinnitus perception.
The limitations of conventional treatments have left many patients searching for more effective solutions. While sound therapies may temporarily mask symptoms and psychological interventions help with coping strategies, neither approach directly targets the aberrant neural activity believed to cause tinnitus. This treatment gap has created significant frustration among both patients and clinicians seeking meaningful interventions for this challenging condition.
Enter neuromodulation—a revolutionary approach that aims to modify the abnormal neural activity patterns responsible for tinnitus perception. Rather than simply masking or managing symptoms, neuromodulation devices intervene at the neurological level, potentially offering a more fundamental solution. These innovative technologies represent a paradigm shift in tinnitus treatment, moving from symptom management toward addressing root causes through targeted neurological intervention.
“Tinnitus is no longer viewed as just an ear problem, but rather a complex neurological condition involving multiple brain regions. Modern treatments must address this neural basis to be truly effective.” – American Tinnitus Association
How Neuromodulation Tackles the Root Cause of Tinnitus
“Unlocking Neuromodulation Therapies” from eremedium.in and used with no modifications.
Neuromodulation represents a fundamental shift in tinnitus treatment philosophy. Instead of simply masking symptoms or teaching patients to cope with persistent noise, these technologies aim to normalize the dysfunctional neural activity patterns that generate tinnitus in the first place. By delivering precisely calibrated stimuli to specific neural pathways, neuromodulation devices can potentially “rewire” the brain’s processing of auditory information, leveraging the brain’s natural neuroplasticity to reduce or eliminate phantom sound perception.
This approach aligns with our modern understanding that tinnitus is primarily a neurological disorder rather than simply an auditory one. By targeting the neural networks involved in tinnitus generation and perception, neuromodulation offers the possibility of more profound and lasting relief than conventional symptom-focused treatments. The Neuromod approach exemplifies this shift toward addressing fundamental neurological mechanisms rather than superficial symptom management.
The Neurological Basis of Tinnitus
To understand how neuromodulation works, we must first comprehend the neural mechanisms underlying tinnitus. While often triggered by hearing damage, tinnitus typically persists due to maladaptive changes in how the brain processes auditory information. When sensory hair cells in the inner ear are damaged, they stop sending normal signals to the brain. The brain compensates for this reduced input by increasing its sensitivity, essentially “turning up the gain” on remaining signals.
This neural hyperactivity creates abnormal firing patterns in auditory pathways and associated brain regions, including the auditory cortex, limbic system, and areas involved in attention and emotional processing. These disrupted patterns manifest as the phantom sounds experienced in tinnitus. Brain imaging studies have confirmed structural and functional changes in multiple brain regions in tinnitus patients, demonstrating that it’s truly a “brain disorder” rather than just an “ear problem.”
Importantly, these maladaptive neural changes often become self-sustaining even after the initial trigger is gone. The brain essentially “learns” these dysfunctional patterns through neuroplasticity—the same mechanism that allows us to acquire new skills but can unfortunately also reinforce harmful patterns. This understanding explains why tinnitus often persists indefinitely and why traditional treatments focusing solely on the auditory system have limited effectiveness.
| Brain Region | Normal Function | Changes in Tinnitus |
|---|---|---|
| Auditory Cortex | Sound processing | Hyperactivity and reorganization |
| Limbic System | Emotional response | Heightened stress response to phantom sounds |
| Frontal Lobe | Attention control | Difficulty filtering out tinnitus perception |
What Neuromodulation Actually Does in the Brain
Neuromodulation devices work by delivering carefully calibrated stimuli that can disrupt and potentially normalize the dysfunctional neural activity patterns responsible for tinnitus. These interventions leverage the brain’s neuroplasticity—its ability to reorganize itself by forming new neural connections. By repeatedly pairing specific stimuli (such as sounds and gentle electrical pulses), neuromodulation can essentially “teach” the brain to reduce its hyperactivity in the auditory processing pathways and associated regions.
FDA-Approved Devices Transforming Tinnitus Treatment
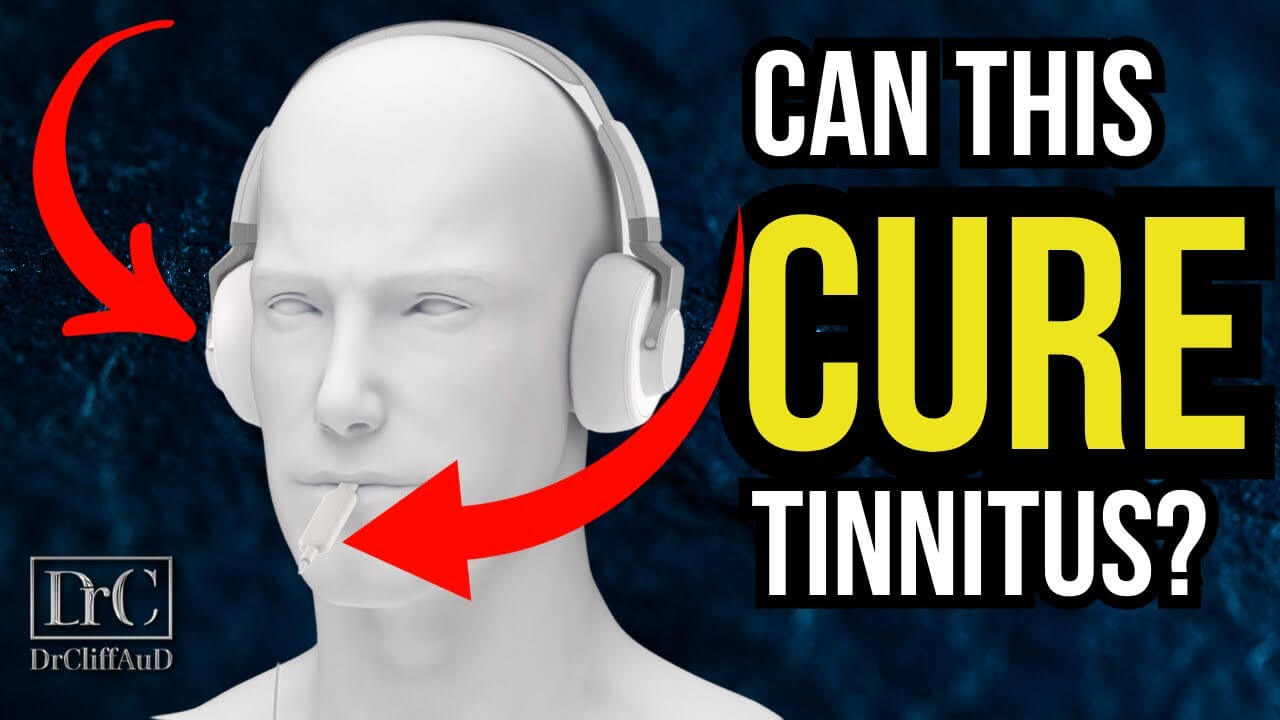
“Lenire: A New Era in Tinnitus Treatment …” from www.youtube.com and used with no modifications.
The landscape of tinnitus treatment changed dramatically in March 2023 when the FDA granted clearance to the first neuromodulation device specifically designed for tinnitus management. This milestone marked the beginning of a new era in tinnitus care, offering evidence-based options beyond traditional approaches. The approval came after rigorous clinical testing and represents a significant advancement in our ability to address this challenging condition.
Regulatory clearance has opened doors for patients who previously had limited treatment options. With formal FDA recognition, these devices have moved from experimental status to legitimate medical interventions that clinicians can confidently recommend. This shift has also facilitated greater insurance coverage consideration and increased accessibility for patients seeking relief from chronic tinnitus.
Lenire: The First FDA-Approved Bimodal Neuromodulation System
The Lenire system, developed by Neuromod Devices, stands as the pioneering FDA-approved bimodal neuromodulation device specifically designed for tinnitus management. This breakthrough technology combines two forms of simultaneous stimulation: audio tones delivered through headphones and mild electrical stimulation applied to the tongue via a small device called the Tonguetip®. This dual-stimulation approach is based on the principle that synchronized activation of multiple sensory pathways can drive more profound neuroplastic changes than single-modality approaches.
Supported by extensive research including the landmark TENT-A clinical trial series involving over 500 patients, Lenire has demonstrated both safety and efficacy. The system’s development represents years of scientific investigation into the neurological underpinnings of tinnitus and practical applications of neuroplasticity principles. Its FDA clearance in 2023 marked a watershed moment for tinnitus patients seeking evidence-based alternatives to conventional treatments.
How the Lenire Device Works
The Lenire system operates through a precisely coordinated bimodal stimulation protocol. During treatment sessions, patients wear headphones that deliver a customized sequence of tones while simultaneously using the Tonguetip® device, which provides gentle electrical stimulation to specific areas of the tongue. The tongue serves as an ideal stimulation target due to its rich sensory innervation and direct pathways to brain regions involved in sensory integration.
This synchronized stimulation is thought to drive neuroplastic changes in the brain by activating multiple sensory pathways simultaneously. The protocol typically involves daily 30-60 minute sessions over a 12-week period, with the specific stimulation parameters personalized to each patient’s tinnitus characteristics. Treatment can be self-administered at home after initial setup and training by a healthcare professional, making it convenient for long-term use.
The underlying mechanism involves targeting the auditory system while simultaneously stimulating the somatosensory pathway through the trigeminal nerve. This paired stimulation approach appears to reset the abnormal neural synchrony associated with tinnitus perception, potentially through a process known as “spike-timing-dependent plasticity.” By repeatedly pairing these stimuli, the brain gradually “unlearns” the maladaptive patterns responsible for tinnitus.
Clinical Evidence from TENT-A Studies
The Treatment Evaluation of Neuromodulation for Tinnitus (TENT-A) clinical trial series provides the most comprehensive evidence for bimodal neuromodulation efficacy. The initial TENT-A1 study demonstrated that approximately 80% of participants experienced statistically significant improvements in tinnitus symptoms following a 12-week treatment period. More impressively, TENT-A2 showed that these benefits persisted for up to 12 months after treatment completion, suggesting that neuromodulation induces lasting neuroplastic changes rather than merely temporary relief.
The TENT-A3 study further validated these findings while exploring optimal treatment protocols. Across all studies, approximately 70.3% of participants reported meaningful improvement in their tinnitus symptoms, with minimal side effects reported. These results represent some of the most promising clinical outcomes in the tinnitus treatment literature and establish bimodal neuromodulation as a legitimate frontline intervention for chronic tinnitus.
“The results from our clinical trials demonstrate that combined auditory and somatosensory stimulation delivered in a coordinated manner can yield significant improvements in tinnitus severity.” – TENT-A Research Team
Other Neuromodulation Technologies for Tinnitus
“Lenire: The New Tinnitus Treatment” from hearingup.com and used with no modifications.
Transcranial Magnetic Stimulation (TMS)
Transcranial Magnetic Stimulation represents another promising approach to tinnitus neuromodulation. This non-invasive technique uses powerful electromagnetic fields to stimulate specific brain regions, particularly the auditory cortex where much of the aberrant activity associated with tinnitus originates. By applying rapid magnetic pulses through a coil placed against the scalp, TMS can temporarily disrupt or modulate neural activity patterns believed to generate tinnitus perception.
Research on TMS for tinnitus shows varying degrees of effectiveness, with some studies reporting significant but often temporary reductions in tinnitus perception. Different protocols exist, including repetitive TMS (rTMS) which delivers multiple pulses in succession to induce longer-lasting effects. While not yet FDA-approved specifically for tinnitus, TMS has established safety profiles from its approved uses in depression and other neurological conditions, making it an active area of clinical investigation for tinnitus management.
Deep Brain Stimulation
Deep Brain Stimulation (DBS) represents one of the more invasive neuromodulation approaches being investigated for severe, treatment-resistant tinnitus. This technique involves surgically implanting electrodes into specific brain regions, connected to an implantable pulse generator similar to a pacemaker. The electrodes deliver precise electrical stimulation to target areas involved in tinnitus generation or perception, such as the auditory cortex or specific thalamic nuclei. For those interested in understanding more about the underlying mechanisms, exploring how neuroplasticity impacts tinnitus can provide valuable insights.
Due to its invasive nature, DBS for tinnitus remains primarily investigational and is typically considered only for the most severe and debilitating cases. Early research has shown promising results in small case series, with some patients experiencing substantial tinnitus reduction. However, the surgical risks, potential complications, and irreversibility of the procedure necessitate careful patient selection and further research before widespread clinical application. For those seeking alternative treatments, Progressive Tinnitus Management may offer a non-invasive option.
Current DBS research for tinnitus focuses on refining target selection, optimizing stimulation parameters, and identifying predictive factors for treatment success. As our understanding of the neural circuits involved in tinnitus advances, DBS protocols continue to evolve, potentially offering hope for patients with the most severe and refractory forms of tinnitus.
Vagus Nerve Stimulation
Vagus Nerve Stimulation (VNS) represents an innovative neuromodulation approach that pairs electrical stimulation of the vagus nerve with specific auditory stimuli. This technique leverages the vagus nerve’s wide-ranging connections throughout the body and brain, including pathways that influence neuroplasticity and sensory processing. In tinnitus applications, VNS typically involves delivering brief electrical pulses to the vagus nerve (either through an implanted device or transcutaneously) while simultaneously presenting therapeutic sounds designed to counteract tinnitus.
The theoretical basis for VNS in tinnitus treatment centers on the nerve’s ability to trigger release of neurochemicals like acetylcholine and norepinephrine, which facilitate neuroplastic changes. By pairing this neuromodulatory effect with targeted auditory stimulation, VNS aims to reverse the maladaptive neural patterns underlying tinnitus perception. Early clinical studies have shown promising results in subgroups of tinnitus patients, though more extensive research is needed to establish optimal protocols and predictors of treatment response.
Spinal Cord Stimulation
Spinal Cord Stimulation (SCS) represents one of the more exploratory approaches to tinnitus neuromodulation. This technique, which has established applications in chronic pain management, involves implanting electrodes near the spinal cord to modulate neural signaling. For tinnitus applications, researchers have investigated whether stimulating certain spinal pathways might influence auditory processing through ascending connections to the brain, potentially disrupting the aberrant neural activity responsible for tinnitus perception. Learn more about progressive tinnitus management and its potential benefits.
While still in early investigational stages for tinnitus specifically, some case reports and small studies have suggested potential benefit in patients with both tinnitus and certain forms of somatosensory involvement. SCS might be particularly relevant for patients whose tinnitus is influenced by head, neck, or jaw movements, suggesting a somatosensory component. As with other invasive approaches, SCS requires careful consideration of risk-benefit profiles and remains primarily in the research domain for tinnitus applications. For those exploring non-invasive options, Progressive Tinnitus Management offers a structured approach to managing symptoms.
What the Research Shows: Effectiveness and Limitations
“Closing in on tinnitus treatments …” from www.health.harvard.edu and used with no modifications.
The scientific evidence supporting neuromodulation for tinnitus has grown substantially in recent years, with multiple well-designed clinical trials demonstrating meaningful benefits. The most robust data comes from the TENT-A trial series, which collectively enrolled over 500 participants across three separate studies. These trials consistently showed that approximately 70-80% of patients experienced clinically significant improvement in tinnitus symptoms following a 12-week bimodal neuromodulation protocol.
Perhaps most encouragingly, follow-up assessments have demonstrated that these benefits persist long after the initial treatment period. The TENT-A2 study found that improvements were maintained for 12 months post-treatment, suggesting that neuromodulation induces lasting neuroplastic changes rather than temporary symptomatic relief. This durability of effect represents a significant advantage over many conventional tinnitus treatments, which often require ongoing use to maintain benefits.
Despite these promising results, it’s important to acknowledge the limitations of current evidence. Not all patients respond equally to neuromodulation, and researchers are still working to identify reliable predictors of treatment success. Additionally, most studies have focused on subjective outcome measures like tinnitus questionnaires rather than objective biomarkers, reflecting the inherently subjective nature of tinnitus perception.
Success Rates from Clinical Trials
Clinical trials of bimodal neuromodulation have consistently demonstrated impressive response rates. In the pivotal TENT-A2 study, 70.3% of participants reported meaningful improvement in tinnitus symptoms after completing the 12-week treatment protocol. More remarkably, these benefits persisted during follow-up assessments, with minimal regression even at the 12-month mark. This suggests that neuromodulation may induce lasting neuroplastic changes that fundamentally alter tinnitus perception pathways.
Different neuromodulation approaches show varying efficacy profiles. While bimodal stimulation (combining auditory and somatosensory stimulation) has the strongest evidence base, other techniques like transcranial magnetic stimulation typically show more modest and variable results. TMS studies report response rates ranging from 25-60% depending on the specific protocol and patient population, with effects often being more temporary than those seen with bimodal approaches.
Importantly, even within successful trials, the degree of improvement varies considerably between individuals. Some patients experience dramatic reduction in tinnitus perception, while others note more modest benefits. This variability highlights the heterogeneous nature of tinnitus and underscores the need for personalized treatment approaches that can be tailored to individual pathophysiology.
Who Benefits Most from Neuromodulation
Research suggests that several factors may influence response to neuromodulation treatments. Duration of tinnitus appears significant, with some studies indicating better outcomes in patients whose tinnitus has been present for less than 10 years, possibly reflecting greater neural plasticity in more recent cases. The specific qualities of a patient’s tinnitus also matter—those with tonal (single-frequency) tinnitus tend to respond better than those with more complex noise patterns.
Age may also play a role in treatment response, though findings have been inconsistent across studies. Some research suggests younger patients may show greater improvement, potentially due to enhanced neuroplasticity, while other studies find no significant age-related differences. Hearing status represents another important consideration, with varying responses observed between patients with normal hearing versus those with significant hearing loss.
Psychological factors should not be overlooked when predicting treatment outcomes. Patients with lower baseline anxiety and depression scores often demonstrate better response to neuromodulation. This may reflect the complex bidirectional relationship between tinnitus perception and emotional state, with each potentially amplifying the other. Motivation and treatment adherence also significantly impact outcomes, as consistent daily use appears crucial for optimal results. For more insights, explore how neuroplasticity impacts tinnitus and emotional well-being.
Types of Tinnitus That Respond to Treatment
Neuromodulation appears particularly effective for tinnitus with specific characteristics. Somatic tinnitus—where symptoms can be temporarily modified by head, neck, or jaw movements—often responds well to bimodal stimulation approaches that include somatosensory elements. This likely reflects the involvement of cross-modal neural pathways between auditory and somatosensory systems in these patients.
Patients with bilateral tinnitus (affecting both ears) generally show good response rates to neuromodulation, though some studies suggest unilateral cases may experience even greater improvement. The tonal quality of tinnitus also appears relevant, with pure-tone tinnitus often responding better than broadband noise patterns. This may reflect differences in the underlying neural circuits generating these distinct perceptual experiences.
Importantly, neuromodulation appears effective regardless of tinnitus etiology in many cases. Whether the initial trigger was noise exposure, ototoxic medications, head trauma, or idiopathic causes, the treatment can still yield benefits if the underlying neural mechanisms involve the pathways targeted by the specific neuromodulation approach. This broad applicability makes neuromodulation particularly valuable given the diverse origins of tinnitus in the clinical population.
Getting Started with Neuromodulation Treatment
“Neuromodulation Treatment in Southlake, TX” from www.southlakepainrelief.com and used with no modifications.
For patients considering neuromodulation for tinnitus, the journey typically begins with a comprehensive evaluation by an audiologist or otolaryngologist experienced in tinnitus management. This assessment should include detailed hearing tests, tinnitus characterization (pitch, loudness, quality), and evaluation of potential underlying causes. Specialists may also administer standardized questionnaires to assess tinnitus severity and impact on quality of life, establishing important baseline measurements for tracking treatment progress.
After this initial assessment, appropriate candidates will discuss specific neuromodulation options with their healthcare provider. For FDA-approved devices like Lenire, patients may be referred to a specialized tinnitus center or trained provider who can properly configure the device and provide necessary training. The treatment team will explain the scientific basis of the therapy, set realistic expectations regarding potential outcomes, and outline the commitment required for optimal results.
Patient selection involves careful consideration of several factors. Ideal candidates typically have moderate to severe tinnitus that significantly impacts quality of life, have already tried first-line interventions like sound therapy or hearing aids, and demonstrate sufficient motivation to adhere to the daily treatment protocol. Certain medical conditions or device-specific contraindications may exclude some patients, highlighting the importance of thorough screening and honest discussion about candidacy.
Doctor Consultation and Assessment Process
The initial consultation for neuromodulation typically involves a detailed medical history focused on tinnitus onset, progression, and previous treatments. Clinicians pay particular attention to potential triggers, aggravating factors, and any somatic modulation (changes in tinnitus with body movements). A comprehensive audiological assessment provides crucial information about hearing status and helps characterize the tinnitus through pitch and loudness matching procedures.
Many specialists utilize standardized questionnaires like the Tinnitus Handicap Inventory (THI) or Tinnitus Functional Index (TFI) to quantify symptom severity and impact on quality of life. These validated instruments not only help determine treatment candidacy but also establish baseline measurements for tracking progress. Additional assessments may include evaluating psychological factors like anxiety or depression that often co-occur with tinnitus and may influence treatment outcomes.
Following these assessments, the healthcare provider will discuss whether neuromodulation represents an appropriate treatment option based on the individual’s specific presentation. For suitable candidates, they will explain device options, expected outcomes based on current evidence, and any contraindications or precautions. This collaborative decision-making process ensures patients have realistic expectations and understand their role in the treatment journey.
Insurance Coverage and Out-of-Pocket Costs
As a relatively new treatment modality, insurance coverage for neuromodulation devices varies considerably across providers and plans. Since FDA clearance in 2023, more insurance companies have begun evaluating coverage policies for devices like Lenire, though many still classify these treatments as investigational or experimental. Patients should work directly with their healthcare providers and device manufacturers to determine potential coverage options, including possible prior authorization requirements or medical necessity documentation.
What to Expect During Treatment
Neuromodulation treatment typically begins with a device fitting and programming session conducted by a trained healthcare professional. For bimodal systems like Lenire, this includes customizing both the audio stimulus profile and the tongue stimulation parameters based on the patient’s specific tinnitus characteristics and comfort thresholds. Patients receive comprehensive training on proper device use, including electrode placement, stimulation intensity adjustment, and troubleshooting common issues. To understand more about the methods used in tinnitus management, you can explore progressive tinnitus management.
The standard treatment protocol involves daily sessions lasting 30-60 minutes, typically conducted at home. Patients use the device while engaged in quiet activities like reading or relaxing, focusing on consistent daily use rather than specific times of day. Many devices include companion apps or software that track usage patterns and compliance, allowing healthcare providers to monitor adherence remotely and make adjustments if needed.
Typical Treatment Duration and Protocols
Based on clinical trial protocols and manufacturer recommendations, the initial treatment course for bimodal neuromodulation typically spans 12 weeks of daily use. This duration aligns with the time needed to induce meaningful neuroplastic changes in brain function based on current understanding of neural adaptation mechanisms. During this period, patients generally use the device for 30-60 minutes per day, with consistent adherence strongly correlated with better outcomes.
Following the initial treatment phase, protocols may vary based on individual response. Some patients benefit from continued regular use, while others maintain improvements with reduced frequency “maintenance” sessions. The TENT-A2 study demonstrated that many patients maintain benefits for 12 months after completing the initial protocol, suggesting that periodic “booster” treatments might be sufficient for long-term management rather than indefinite daily use.
Frequently Asked Questions
Patients considering neuromodulation treatment for tinnitus typically have numerous questions about what to expect. The following section addresses the most common inquiries based on current clinical evidence and practical experience. Understanding these aspects can help individuals make informed decisions about whether this treatment approach aligns with their specific needs and circumstances.
Remember that while these answers reflect general information, individual experiences may vary. It’s always recommended to discuss specific concerns with a qualified healthcare provider who can offer personalized guidance based on your particular tinnitus presentation and medical history.
- What makes neuromodulation different from traditional tinnitus treatments?
- Is neuromodulation painful or uncomfortable?
- How soon after starting treatment might I notice changes in my tinnitus?
- Will my tinnitus return if I stop using the device?
- Can I use neuromodulation if I have a hearing aid or cochlear implant?
These questions reflect common concerns among patients considering this treatment option. The answers provided below are based on current scientific understanding and clinical experience with FDA-approved devices. As research continues to advance, our knowledge about optimal use patterns and expected outcomes will continue to evolve.
How long does it take to see results from neuromodulation treatment for tinnitus?
Response timelines vary significantly between individuals, but most patients who benefit from neuromodulation begin noticing changes within 2-6 weeks of consistent daily use. Some report subtle improvements in tinnitus intensity or distress within the first few weeks, while others experience more gradual changes that become apparent toward the end of the standard 12-week protocol. It’s important to note that neuroplastic changes typically develop progressively rather than suddenly, so patience and consistent adherence to the treatment regimen are essential for optimal outcomes.
Are neuromodulation devices for tinnitus covered by insurance?
Insurance coverage for neuromodulation devices remains variable following FDA clearance in 2023. Some private insurance plans have begun covering these treatments, particularly for patients with severe, treatment-resistant tinnitus who meet specific criteria. Coverage decisions typically consider factors such as documented failure of conventional treatments, significant impact on quality of life, and adherence to approved protocols under appropriate medical supervision.
For patients without insurance coverage, manufacturers often offer payment plans or financing options to make treatment more accessible. Some practices also provide rental options or trial periods that allow patients to evaluate effectiveness before committing to purchase. It’s advisable to contact both your insurance provider and the device manufacturer directly to understand specific coverage options and potential out-of-pocket costs in your situation.
Can neuromodulation completely eliminate tinnitus symptoms?
Complete elimination of tinnitus occurs in a minority of patients—approximately 15-20% according to clinical trial data. More commonly, successful treatment results in significant reduction of tinnitus intensity and distress rather than complete silence. Many patients report their tinnitus becomes less intrusive, easier to ignore, and less emotionally disturbing following treatment, even if the perception remains detectable under quiet conditions.
The clinical goal of neuromodulation is typically considered improvement in quality of life and reduction in tinnitus-related distress rather than complete symptom elimination. Most patients who respond positively to treatment experience meaningful improvements in sleep, concentration, emotional well-being, and daily functioning, even if some level of tinnitus perception persists. These functional improvements often represent more important outcomes than changes in the acoustic properties of the tinnitus itself.
Are there any side effects from using neuromodulation devices?
Neuromodulation devices for tinnitus have demonstrated excellent safety profiles in clinical trials, with side effects typically being mild and temporary. For bimodal devices like Lenire, the most commonly reported side effects include temporary tingling or metallic taste sensations during tongue stimulation, minor discomfort at the stimulation site, and occasional headaches especially during initial use. These effects are generally well-tolerated and often diminish as patients become accustomed to the treatment.
Importantly, clinical trials have not identified any serious adverse effects associated with FDA-approved devices when used as directed. There is no evidence that properly administered neuromodulation worsens tinnitus or causes permanent changes in sensation or function. As with any medical device, patients should promptly report any unexpected or concerning symptoms to their healthcare provider for appropriate evaluation and management.
Can I use neuromodulation alongside other tinnitus treatments?
Neuromodulation can generally be safely combined with most conventional tinnitus management approaches, potentially offering synergistic benefits. Many patients successfully use neuromodulation alongside hearing aids, sound therapy, cognitive behavioral therapy, or tinnitus retraining therapy. The multifaceted nature of tinnitus often benefits from this comprehensive approach, addressing both the neurological aspects through neuromodulation and the psychological or functional components through complementary interventions.
When considering combination therapy, it’s important to coordinate care between all involved healthcare providers to ensure treatments complement rather than conflict with each other. Some specific interventions may need scheduling adjustments to avoid interference—for example, separating neuromodulation sessions from certain sound therapy protocols. Your tinnitus management team can help develop an integrated treatment plan that maximizes benefits while minimizing potential conflicts between approaches.
For patients with complex tinnitus presentations or multiple contributing factors, this multimodal approach often yields the best outcomes. By addressing the condition from multiple angles simultaneously, combination therapy can tackle various aspects of tinnitus generation and perception, potentially offering more comprehensive relief than any single intervention alone. Neuromodulation for tinnitus continues to lead the way in developing innovative solutions that can work alongside traditional tinnitus management approaches.