Article-At-A-Glance
- No FDA-approved medications specifically treat tinnitus, though some medications may help manage related symptoms or underlying causes
- Antidepressants and anti-anxiety medications can provide relief for some patients by addressing emotional distress associated with tinnitus
- Over-the-counter supplements like melatonin and zinc show mixed results in clinical studies but may benefit specific patient groups
- Combination approaches that pair medications with sound therapy or cognitive behavioral therapy often yield better results than medication alone
- Some medications can actually worsen tinnitus symptoms, making it crucial to consult with a healthcare provider before starting any treatment
The Reality of Tinnitus: Why Medications Aren’t a Complete Cure

That persistent ringing, buzzing, or hissing in your ears can drive anyone to desperately seek relief. If you’re one of the estimated 50 million Americans suffering from tinnitus, you’ve likely searched for medications that might silence those phantom sounds. The challenging truth is that despite decades of research, no single medication has emerged as a definitive cure for tinnitus. This is largely because tinnitus isn’t a disease itself but a symptom with dozens of potential causes—from hearing loss and ear infections to medication side effects and circulatory problems.
Natural Remedies Guide has been researching tinnitus treatments for over a decade, finding that a comprehensive approach often works better than relying solely on medications. Most treatment protocols now focus on managing the perception of tinnitus rather than eliminating the sound completely. The distinction is crucial—while we may not be able to turn off the ringing, we can potentially change how your brain processes and responds to it.
Understanding this reality sets appropriate expectations as we explore medication options. Think of tinnitus medications not as silver bullets but as potential tools in a more comprehensive treatment strategy. Some may help by targeting underlying causes, while others aim to reduce the distress associated with the condition. Let’s examine what science tells us about these pharmaceutical approaches, separating evidence-based options from wishful thinking.
Tinnitus by the Numbers
– 50 million: Americans with tinnitus
– 20 million: Those with burdensome chronic tinnitus
– 2 million: People with extreme, debilitating cases
– 200+: Medications that list tinnitus as a potential side effect
– 0: FDA-approved medications specifically for tinnitus
FDA-Approved Medications for Tinnitus

“Pain Medicine Could Raise Tinnitus Risk” from www.aarp.org and used with no modifications.
When patients first seek treatment for tinnitus, many are surprised to learn a hard truth about the current pharmaceutical landscape. Despite the prevalence of this condition and decades of research, the medication options specifically approved for tinnitus remain extremely limited.
The Truth: No Direct FDA Approvals
The stark reality is that no medications currently hold FDA approval specifically for treating tinnitus as their primary indication. This doesn’t mean medications aren’t used—they certainly are—but rather that none have satisfied the rigorous clinical trial requirements needed to secure official approval for this specific purpose. The lack of FDA-approved options reflects both the complexity of tinnitus as a symptom and the challenges researchers face in designing studies that can objectively measure tinnitus relief, which remains largely subjective. For more insights on managing tinnitus, you might explore tinnitus management options.
This absence of approved medications isn’t for lack of trying. Numerous pharmaceutical companies have invested in tinnitus research, but the heterogeneous nature of the condition makes it difficult to develop a one-size-fits-all solution. Tinnitus can stem from so many different underlying causes that finding a single compound effective across all cases has proven elusive. Additionally, the subjective nature of tinnitus makes measuring improvement in clinical trials particularly challenging.
Off-Label Prescriptions That Doctors Actually Use
Despite the lack of specific FDA approvals, physicians regularly prescribe numerous medications “off-label” to help manage tinnitus symptoms. Off-label prescribing refers to using FDA-approved medications for conditions other than those they were officially approved to treat. This practice is legal, common, and often based on clinical experience and smaller studies suggesting benefit.
The most commonly prescribed off-label medications for tinnitus include antidepressants (particularly tricyclics like nortriptyline and amitriptyline), anti-anxiety medications (such as alprazolam), anticonvulsants (including gabapentin and carbamazepine), and certain blood flow medications. These aren’t prescribed indiscriminately—doctors typically select medications based on the suspected underlying cause of your tinnitus or its most troublesome associated symptoms.
For instance, if your tinnitus appears related to a vascular condition, medications that improve blood flow might be suggested. If anxiety and sleep disturbances are major components of your tinnitus experience, an antidepressant or anti-anxiety medication might be more appropriate. The key is that these prescribing decisions should be tailored to your specific situation rather than following a standard protocol. For more insights, you might want to explore pine bark extract for tinnitus as a potential management option.
Antidepressants for Tinnitus Relief
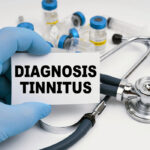
“Antidepressant Side Effects: The Long …” from addictionresource.com and used with no modifications.
Antidepressants represent one of the most commonly prescribed medication classes for tinnitus management, despite not being specifically approved for this purpose. Their use stems from the strong connection between tinnitus perception and neurological processing, particularly in the brain’s emotional centers. Many patients experience significant improvement in tinnitus symptoms when their underlying anxiety or depression is addressed.
How Tricyclic Antidepressants Affect Tinnitus Perception
Tricyclic antidepressants (TCAs) like amitriptyline, nortriptyline, and desipramine often emerge as first-line options for tinnitus treatment among antidepressants. These medications work by increasing levels of neurotransmitters like serotonin and norepinephrine in the brain, which helps modulate the central nervous system’s response to tinnitus. TCAs appear to be particularly helpful for patients whose tinnitus worsens at night or is accompanied by depression, anxiety, or insomnia.
A notable study published in the Journal of Otolaryngology found that approximately 40% of patients experienced at least moderate improvement in their tinnitus symptoms when treated with nortriptyline. Interestingly, this improvement occurred even in patients who didn’t have clinical depression, suggesting these medications may affect tinnitus perception through mechanisms beyond their antidepressant effects. The dosages prescribed for tinnitus are typically lower than those used for depression treatment, often starting at just 10mg daily and gradually increasing as needed.
SSRIs and SNRIs: Effectiveness for Combined Anxiety and Tinnitus
Selective serotonin reuptake inhibitors (SSRIs) like sertraline and fluoxetine, along with serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine, provide another approach for patients struggling with both tinnitus and mood disorders. These newer-generation antidepressants generally have fewer side effects than TCAs, making them more tolerable for many patients. They’re particularly valuable when tinnitus coexists with significant anxiety or depression that independently warrants treatment.
Clinical evidence supporting SSRIs and SNRIs specifically for tinnitus is more mixed than for TCAs. Some studies show modest benefits, while others indicate minimal direct effect on tinnitus perception. However, by alleviating emotional distress, these medications often improve patients’ ability to cope with tinnitus, even if the actual sound perception remains unchanged. The relationship between serotonin regulation and auditory processing continues to be an active area of research that may yield more targeted treatments in the future.
Real Side Effect Concerns You Should Know
While antidepressants can offer significant benefits for tinnitus sufferers, they’re not without potential drawbacks. Common side effects include dry mouth, constipation, blurred vision, and dizziness—with TCAs typically causing more pronounced side effects than SSRIs or SNRIs. Some patients report sexual dysfunction, which can be particularly problematic with SSRIs. Weight gain is another consideration, especially with longer-term use.
More concerning is that some patients actually experience worsening of tinnitus when starting antidepressants. This paradoxical effect seems more common with SSRIs than with TCAs. If you notice your tinnitus intensifying after starting an antidepressant, contact your healthcare provider immediately—don’t simply discontinue the medication, as abrupt cessation can trigger withdrawal symptoms. For more information, you can ask the expert about common tinnitus questions. Most antidepressants require gradual tapering when discontinuing.
The decision to try antidepressants should always involve careful discussion with your healthcare provider about potential benefits versus risks. For many patients with significant tinnitus-related distress, the improvement in quality of life outweighs the manageable side effects. Your provider should monitor you closely during the initial weeks of treatment to assess both benefits and adverse effects.
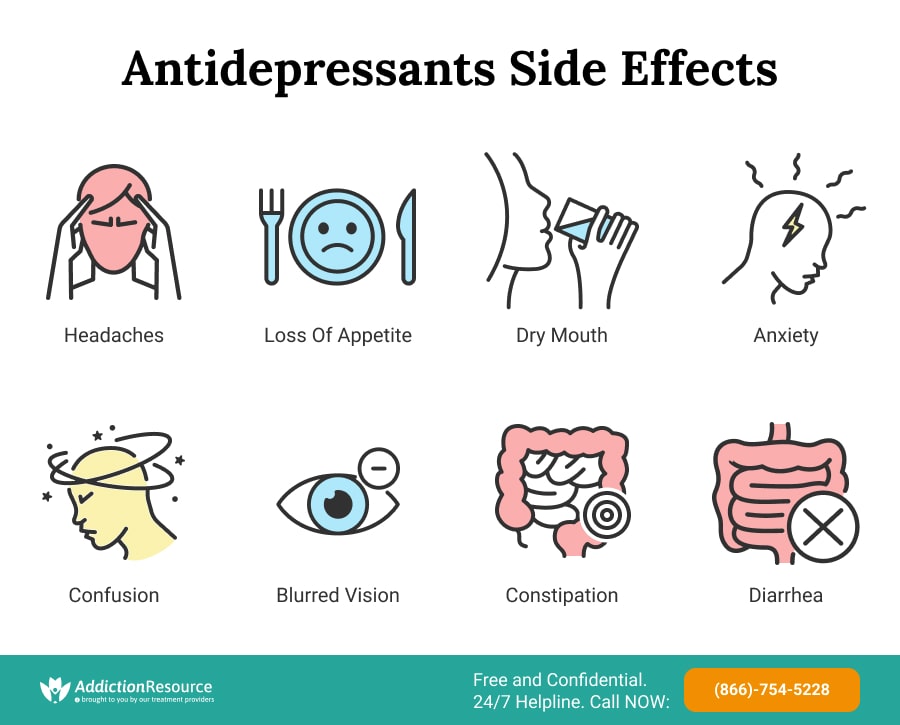
Anti-Anxiety Medications and Their Impact
“Antianxiety Drug Therapy: Video, Causes …” from www.osmosis.org and used with no modifications.
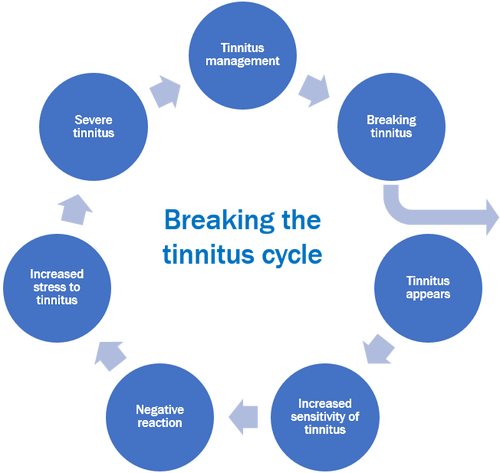
Anxiety and tinnitus often create a vicious cycle—tinnitus causes anxiety, which then makes tinnitus perception worse. Breaking this cycle represents a key strategy in tinnitus management, and anti-anxiety medications can play a valuable role in this approach for some patients. These medications don’t directly reduce the tinnitus sound but may diminish its perceived intensity by addressing the emotional response it triggers. For more information on tinnitus treatment options, visit this helpful guide.
Benzodiazepines: Short-Term Benefits vs. Long-Term Risks
Benzodiazepines like alprazolam (Xanax), clonazepam (Klonopin), and diazepam (Valium) sometimes provide rapid relief for tinnitus-related anxiety and distress. These medications enhance the effect of the inhibitory neurotransmitter GABA in the brain, producing calming effects that can help patients better cope with tinnitus. A small but often-cited study published in the Archives of Otolaryngology found that alprazolam reduced tinnitus severity in 76% of participants, suggesting these medications may actually influence auditory processing beyond just reducing anxiety.
However, the benefits of benzodiazepines come with significant cautions. These medications carry high risks for dependence and tolerance, meaning patients may need increasing doses to achieve the same effect over time. Withdrawal symptoms can be severe and potentially dangerous when discontinuing, particularly after long-term use. Common side effects include drowsiness, cognitive impairment, and coordination problems, which can impact daily functioning. For those seeking alternative treatments, CBD oil for tinnitus relief is an option that some patients explore.
Due to these concerns, most specialists recommend benzodiazepines only for short-term use during particularly difficult periods of tinnitus distress, rather than as a long-term management strategy. If prescribed these medications, work closely with your healthcare provider to use the lowest effective dose for the shortest necessary duration.
Non-Benzodiazepine Options with Fewer Dependency Issues
For patients needing longer-term anxiety management related to tinnitus, several alternatives to benzodiazepines present fewer risks for dependence. Buspirone (BuSpar), which works on serotonin receptors rather than GABA, provides anxiety relief with minimal risk of dependence or withdrawal. Though it takes longer to become effective (typically 2-3 weeks), it doesn’t impair cognition or coordination like benzodiazepines and doesn’t interact with alcohol.
Another approach involves using antidepressants with anxiety-relieving properties, particularly SSRIs and SNRIs as discussed previously. These medications can effectively address anxiety without the dependency concerns of benzodiazepines. Additionally, hydroxyzine, an antihistamine with anxiolytic properties, sometimes helps manage tinnitus-related anxiety, particularly when sleep disturbance is a significant component.
Beta-blockers like propranolol, while not anxiolytics in the traditional sense, can help manage the physical symptoms of anxiety such as rapid heartbeat and trembling. For some tinnitus patients, these physical manifestations of anxiety worsen their perception of tinnitus, making beta-blockers a helpful adjunct therapy in selected cases.
Steroids and Anti-Inflammatories for Tinnitus
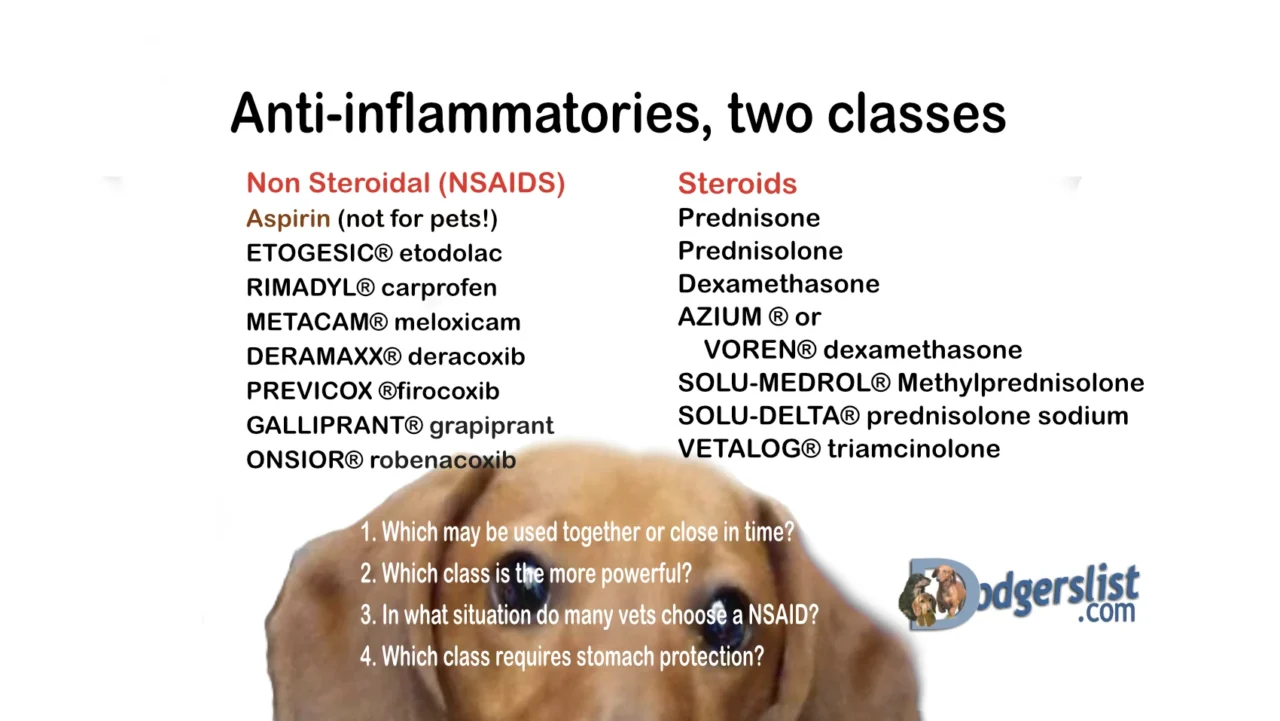
Inflammation plays a surprisingly significant role in many cases of tinnitus, particularly those resulting from inner ear conditions or sudden hearing loss. For these patients, anti-inflammatory medications represent one of the most physiologically direct treatment approaches available. Rather than simply masking symptoms, these medications target what may be an actual underlying cause.
When Inflammation Causes Your Ringing Ears
Inflammatory processes in the inner ear can disrupt normal auditory function and trigger tinnitus. This is especially common in conditions like Meniere’s disease, autoimmune inner ear disease, and sudden sensorineural hearing loss. In these cases, inflammation damages the delicate hair cells and neural connections responsible for sound processing, creating the abnormal neural activity we perceive as tinnitus. When inflammation is the primary culprit, addressing it directly through anti-inflammatory medications can potentially provide substantial relief.
Timing is absolutely critical with inflammatory tinnitus. Research shows that early intervention with anti-inflammatory treatments—ideally within days of symptom onset—yields significantly better outcomes than delayed treatment. This underscores the importance of seeking prompt medical attention for any sudden-onset tinnitus, especially when accompanied by hearing loss, fullness in the ear, or vertigo. For those interested in alternative treatments, exploring options like CBD oil for tinnitus relief might provide additional insights.
Oral vs. Injected Steroids: Which Works Better?
Corticosteroids like prednisone, methylprednisolone, and dexamethasone form the backbone of anti-inflammatory treatment for tinnitus. These potent medications suppress inflammation throughout the body, including in the delicate tissues of the inner ear. For acute tinnitus associated with sudden hearing loss or Meniere’s disease flares, oral steroids typically serve as the first-line treatment, usually in a tapered dosage over 10-14 days.
For patients who don’t respond adequately to oral steroids or who can’t tolerate their systemic side effects, intratympanic steroid injections offer a more targeted alternative. This procedure involves injecting steroid medication directly into the middle ear, where it diffuses into the inner ear through the round window membrane. Studies comparing the two approaches have yielded mixed results, but many specialists now employ a combination strategy—starting with oral steroids and adding intratympanic injections for cases with incomplete response.
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen represent another, milder anti-inflammatory option. While less potent than steroids, they carry fewer side effects and may help manage less severe inflammation-related tinnitus. Some patients report temporary tinnitus relief with NSAIDs, though the evidence for their effectiveness remains largely anecdotal.
Typical Treatment Duration and Expected Results
Anti-inflammatory treatments for tinnitus typically follow a short, intensive course rather than long-term use. Oral steroid regimens usually last 10-14 days, while intratympanic injection protocols often involve 3-4 injections spaced over 1-2 weeks. Extended steroid use carries significant health risks including bone density loss, elevated blood sugar, increased susceptibility to infection, and mood disturbances.
Results from anti-inflammatory treatments vary considerably depending on the underlying cause and timing of intervention. For sudden-onset inflammatory tinnitus treated promptly, success rates can be quite encouraging—studies report 30-60% of patients experience significant improvement. However, long-standing tinnitus rarely responds well to anti-inflammatory treatments, as the initial inflammation has likely resolved and been replaced by permanent changes to auditory processing.
Blood Flow Medications and Vasoactive Substances
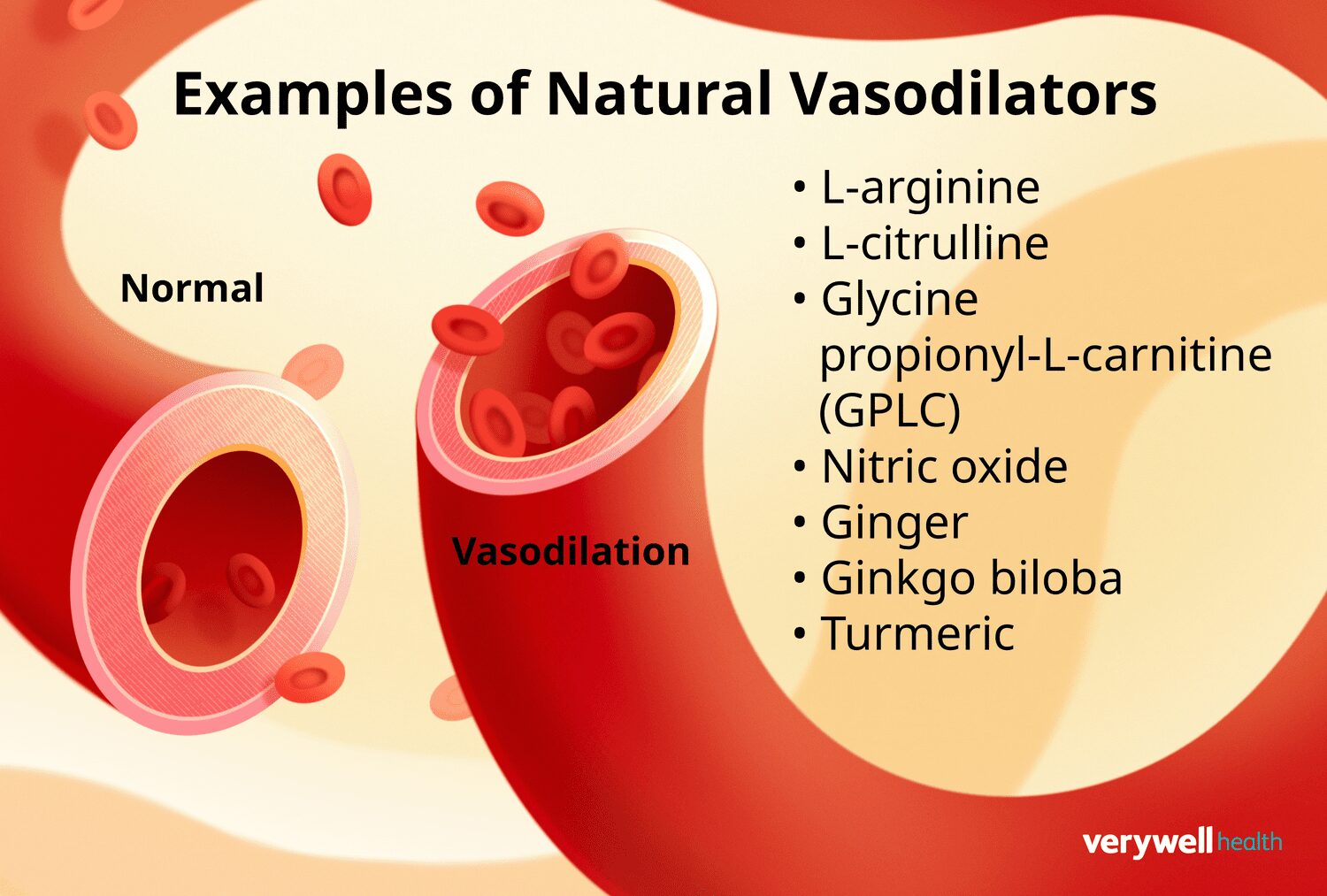
The inner ear’s function depends critically on adequate blood supply, and some cases of tinnitus may stem from compromised microcirculation in this delicate region. This connection has led to interest in medications that improve blood flow as potential tinnitus treatments, particularly for patients with vascular risk factors or whose symptoms worsen with changes in posture or blood pressure.
How Blood Flow Affects Tinnitus Symptoms
The cochlea and vestibular system require exceptional blood supply relative to their small size, making them vulnerable to circulatory problems. Reduced blood flow can starve these structures of oxygen and nutrients, potentially triggering tinnitus through cellular stress responses. This mechanism appears particularly relevant in age-related tinnitus, as microvascular changes and atherosclerosis become more common with advancing years.
Certain tinnitus patterns strongly suggest a vascular component. Pulsatile tinnitus—where the sound beats in rhythm with your heartbeat—often indicates an abnormality in blood vessels near the ear. Similarly, tinnitus that changes with physical exertion, position changes, or carotid compression may have vascular underpinnings. For these specific presentations, medications improving blood flow sometimes provide more targeted relief than other pharmacological approaches.
Evidence Behind Betahistine and Similar Medications
Betahistine, a histamine analog that enhances cochlear blood flow, represents the most widely studied vasoactive medication for tinnitus, particularly in Europe where it’s approved for Meniere’s disease treatment. It works through multiple mechanisms—dilating the small blood vessels supplying the inner ear, reducing endolymphatic pressure, and modulating histamine receptors in the brain. Clinical trials show mixed results, with some studies demonstrating modest benefits for tinnitus patients while others show no significant advantage over placebo.
Other vasoactive medications occasionally prescribed for tinnitus include pentoxifylline, which reduces blood viscosity and improves microcirculation; ginkgo biloba extract, which combines blood flow enhancement with antioxidant properties; and calcium channel blockers like flunarizine, which dilate blood vessels and may regulate neural excitability. Evidence supporting these agents remains limited, though some patients with vascular risk factors report improvement.
Papaverine, nicotinic acid derivatives, and carbogen (a mixture of carbon dioxide and oxygen) represent older approaches to improving cochlear blood flow that have largely fallen out of favor due to limited efficacy and the development of newer alternatives. The search continues for more effective vascular interventions, with novel compounds targeting specific aspects of cochlear blood flow regulation currently under investigation. For those interested in alternative approaches, exploring the use of CBD oil for tinnitus relief could provide additional insights.
Over-the-Counter Options: Separating Facts from Marketing
“Will OTC hearing aids help my tinnitus …” from www.healthyhearing.com and used with no modifications.
The supplement aisles and internet marketplaces overflow with products claiming to relieve or even cure tinnitus. With prescription options limited, many patients turn to these more accessible alternatives. Understanding which have legitimate potential versus those based primarily on marketing hype can save both disappointment and unnecessary expense. For more information on effective treatment options, you can explore this guide on tinnitus treatment options.
Melatonin for Tinnitus-Related Sleep Problems
Sleep disturbance ranks among the most common and distressing tinnitus complications. Melatonin, a hormone that regulates sleep-wake cycles, has shown promise in addressing this specific aspect of tinnitus burden. A randomized controlled trial published in the Annals of Otology, Rhinology, and Laryngology found that 3mg of melatonin taken nightly significantly improved sleep quality in tinnitus patients compared to placebo, with some participants also reporting reduced tinnitus intensity during the day.
Melatonin appears to work through multiple mechanisms relevant to tinnitus. Beyond its sleep-promoting effects, it possesses antioxidant properties that may protect cochlear hair cells and has been shown to modulate auditory processing in the central nervous system. With a favorable safety profile and minimal side effects, melatonin represents one of the more evidence-based supplement options, particularly for tinnitus patients with sleep disturbances. For more information on tinnitus, consider exploring additional resources.
Zinc Supplements: Who Might Actually Benefit
Zinc deficiency can affect nearly every bodily system, including auditory function. Some studies have found links between zinc deficiency and tinnitus, particularly in older adults. A clinical trial published in the American Journal of Otolaryngology reported significant improvement in tinnitus among patients with zinc deficiency when supplemented, while those with normal zinc levels showed minimal benefit.
The evidence suggests a targeted approach to zinc supplementation. Rather than recommending it broadly, testing for zinc deficiency first makes more sense. Populations at higher risk for zinc deficiency who might benefit from testing include elderly individuals, those with malabsorption conditions, vegetarians/vegans, and people taking certain medications like ACE inhibitors or thiazide diuretics. Standard supplementation ranges from 15-30mg daily, with excessive doses potentially causing nausea or altered taste.
Ginkgo Biloba: What the Science Really Shows
Few supplements have been studied as extensively for tinnitus as ginkgo biloba. This herb contains flavonoids and terpenoids that improve microcirculation, provide antioxidant protection, and may modulate neurotransmitter systems. Despite its theoretical promise, clinical trials have yielded conflicting results. A landmark systematic review in the Cochrane Database analyzed 13 randomized controlled trials and concluded that the evidence does not support ginkgo biloba as an effective tinnitus treatment for most patients.
However, the story isn’t quite that simple. Subgroup analyses suggest ginkgo may benefit specific tinnitus populations, particularly those with vascular risk factors or recent-onset symptoms. The typical studied dosage is 120-240mg daily of standardized extract (containing 24% flavonoid glycosides and 6% terpene lactones), with effects potentially taking 4-6 weeks to manifest. Given its generally favorable safety profile, some specialists consider a time-limited trial reasonable for patients with vascular-type tinnitus who understand the limited evidence base.
Lipoflavonoids and Other Heavily Marketed Products
Walk through any pharmacy or browse online tinnitus forums, and you’ll encounter numerous proprietary formulations marketed specifically for tinnitus relief. Lipoflavonoids, perhaps the most heavily advertised, contain lemon bioflavonoids along with vitamins including B12 and C. Despite decades on the market and compelling testimonials, independent clinical research supporting these products remains sparse. The few published studies have methodological limitations including small sample sizes and lack of appropriate controls.
Other commonly marketed supplements include vinpocetine, coenzyme Q10, pine bark extract, garlic, and magnesium. While each has theoretical mechanisms that could benefit tinnitus, robust clinical evidence for their efficacy remains limited. This doesn’t necessarily mean these supplements are ineffective—many simply haven’t been adequately studied in well-designed trials. When considering such products, maintain realistic expectations and ideally discuss with a healthcare provider familiar with supplement research.
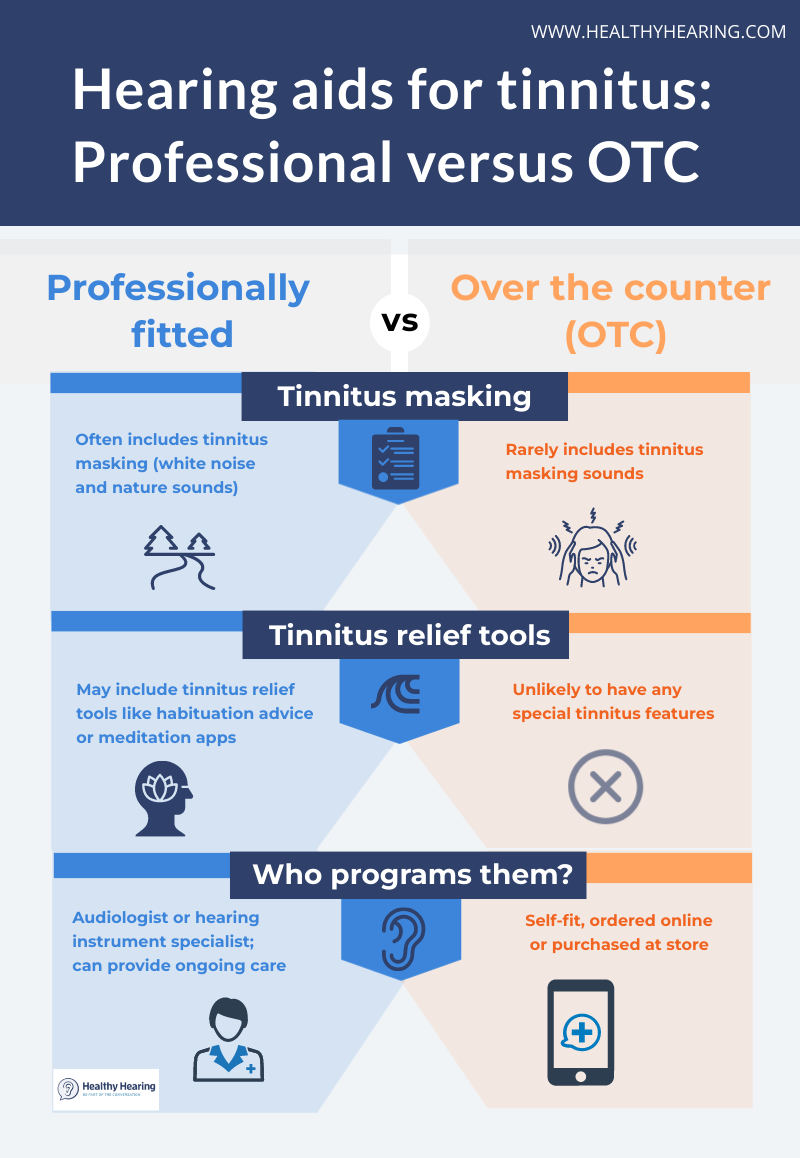
Pairing Medications with Sound Therapy
The most effective tinnitus treatment approaches often combine pharmaceutical interventions with sound therapy techniques. Sound therapy works by introducing external sounds that can mask, distract from, or desensitize you to tinnitus. When paired with appropriate medications, these acoustic strategies often yield better results than either approach alone. Simple forms include using white noise machines, fans, or smartphone apps that generate soothing background sounds, while more sophisticated options involve wearable sound generators or hearing aids with built-in masking features.
Cognitive Behavioral Therapy Plus Medication
Cognitive Behavioral Therapy (CBT) has emerged as one of the most effective tinnitus interventions, helping patients change their emotional and cognitive responses to tinnitus. When combined with appropriate medications, this dual approach addresses both the neurophysiological and psychological aspects of tinnitus distress. For example, an antidepressant might help regulate neurotransmitter systems while CBT provides practical coping strategies and thought restructuring techniques. Research shows this combination often produces greater quality-of-life improvements than medication alone, particularly for patients with significant tinnitus-related distress.
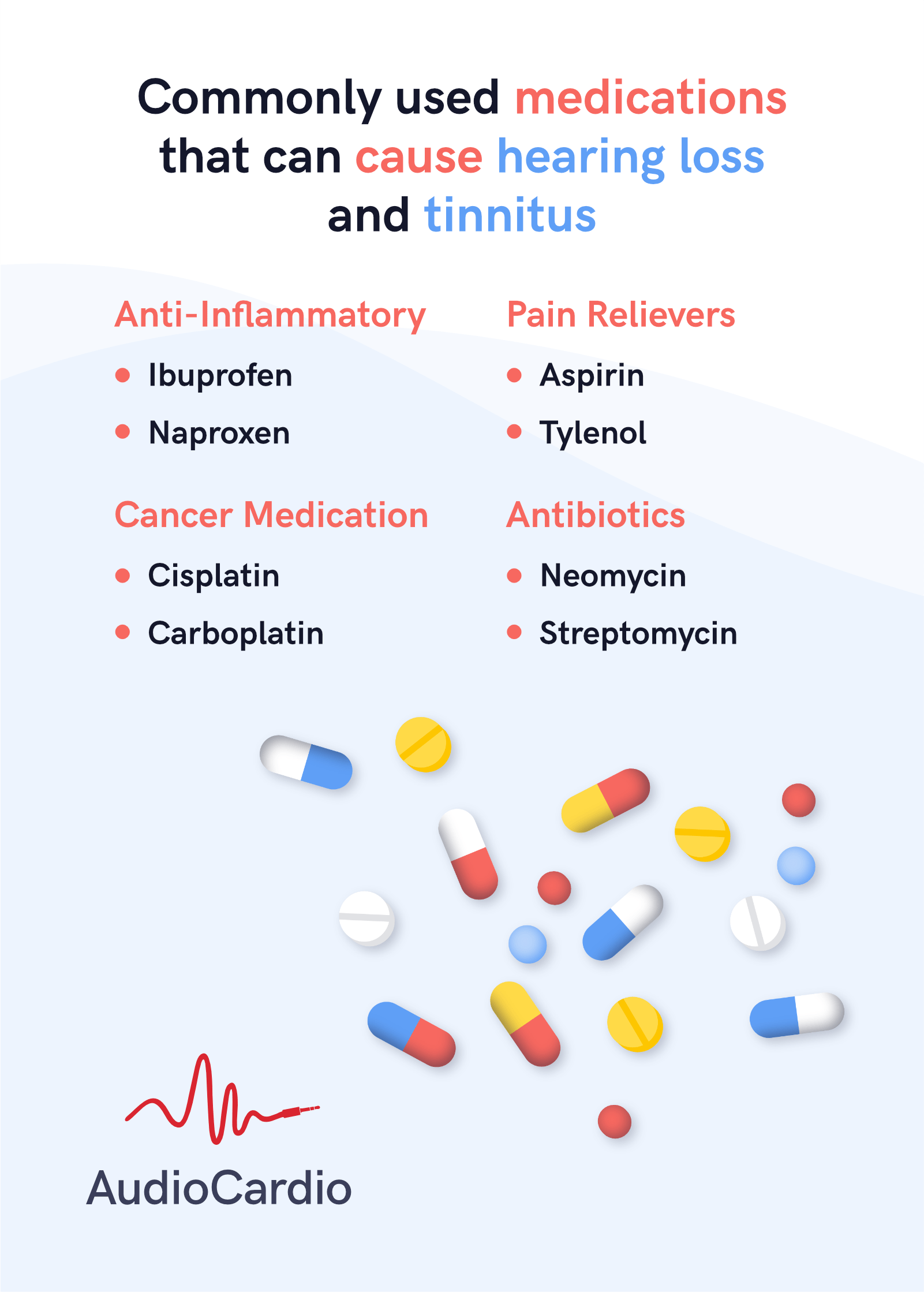
When Medications Can Make Tinnitus Worse
“Medications That Can Cause Hearing Loss …” from audiocardio.com and used with no modifications.
While we’ve explored medications that might help tinnitus, it’s equally important to understand that some medications can actually cause or worsen this condition. Drug-induced tinnitus, technically termed ototoxicity, occurs when medications damage the sensory cells or neural connections in the auditory system. This damage can trigger new tinnitus or exacerbate existing symptoms, sometimes permanently. For alternative approaches, some individuals explore options like acupuncture for tinnitus to manage their symptoms.
The risk varies widely between medications and individuals. Factors influencing susceptibility include dosage, duration of treatment, concurrent kidney or liver disease, age, genetic factors, and pre-existing hearing or ear conditions. Some patients experience tinnitus after just a single dose of an ototoxic medication, while others can take the same drug for years without auditory effects.
- Aspirin and NSAIDs in high doses (temporary and typically reversible)
- Certain antibiotics, particularly aminoglycosides like gentamicin and streptomycin
- Loop diuretics such as furosemide and bumetanide
- Some chemotherapy agents, especially platinum-based drugs like cisplatin
- Quinine-based medications (including some antimalarials)
- Certain antidepressants, particularly some SSRIs
The relationship between medications and tinnitus isn’t always straightforward. Sometimes the connection is obvious—tinnitus begins shortly after starting a new medication and resolves when it’s discontinued. In other cases, the onset is gradual or delayed, making the association harder to identify. Additionally, some medications contribute to tinnitus through indirect mechanisms like altering blood pressure or fluid balance rather than through direct ototoxicity.
Never stop taking a prescribed medication without consulting your healthcare provider, even if you suspect it’s contributing to your tinnitus. Abrupt discontinuation of many medications can cause serious health consequences that may outweigh the tinnitus symptoms. Instead, discuss your concerns with your provider, who can help evaluate whether the medication is likely responsible and explore alternative treatments.
Ototoxic Medications to Avoid
Among ototoxic medications, certain classes carry particularly high risks for tinnitus and should be approached with caution if you already experience this symptom. Aminoglycoside antibiotics like gentamicin can cause permanent damage to inner ear hair cells, especially with prolonged use or high doses. Platinum-based chemotherapy agents, particularly cisplatin, rank among the most consistently ototoxic medications, with studies indicating 40-80% of patients develop some degree of hearing loss or tinnitus. High-dose salicylates (including aspirin when taken at anti-inflammatory doses exceeding 12 tablets daily) frequently cause temporary tinnitus through effects on cochlear function and auditory neural activity. When these or other known ototoxic medications are medically necessary, careful monitoring and potential protective strategies become essential.
How to Talk to Your Doctor About Medication Concerns
Approaching medication concerns effectively requires preparation and clear communication. Before your appointment, document your tinnitus symptoms in detail—when they started, how they’ve changed, and any patterns you’ve noticed in relation to medication use. Create a comprehensive list of all medications you take, including over-the-counter products, supplements, and occasional medications. During the conversation, ask specific questions about whether your current medications might affect tinnitus and what alternatives might exist with lower ototoxicity risks. If your provider dismisses legitimate concerns without adequate explanation, consider seeking a second opinion, ideally from an otolaryngologist or audiologist specializing in tinnitus management.
Finding Your Best Treatment Path Forward
“Tinnitus Clinic Sydney | Hearing Aids …” from hearingaidsprofessionals.com.au and used with no modifications.
The journey to effective tinnitus management rarely follows a straight line. Most patients need to try multiple approaches before finding their optimal treatment combination. Begin by identifying specialist providers knowledgeable about current tinnitus research—typically audiologists, otolaryngologists, or neurologists with specific interest in this condition. These specialists can provide comprehensive evaluation to identify any underlying treatable causes and guide you through evidence-based options based on your specific tinnitus characteristics and overall health profile.
Remember that patience and persistence matter enormously in tinnitus treatment. Many interventions require weeks or even months to show their full benefit. Keep detailed records of treatments tried, their effects (both positive and negative), and how your symptoms respond over time. This documentation proves invaluable in refining your treatment approach. Perhaps most importantly, maintain realistic expectations—while complete elimination of tinnitus isn’t always possible with current medical knowledge, significant improvement in symptoms and their impact on your quality of life remains an achievable goal for most patients with the right combination of treatments, such as using Starkey Livio AI.
Frequently Asked Questions
Tinnitus medication questions represent some of the most common concerns patients bring to healthcare providers. Understanding the answers to these frequently asked questions can help set realistic expectations and guide treatment decisions. While individual responses to medications vary considerably, these evidence-based answers provide general guidance for tinnitus sufferers considering pharmaceutical options.
- What’s the difference between tinnitus treatments and cures?
- How do I know if my tinnitus is temporary or permanent?
- Should I try multiple medications simultaneously?
- What should I do if my tinnitus suddenly worsens?
- Can children and elderly patients take the same tinnitus medications?
Remember that medication represents just one aspect of comprehensive tinnitus management. Sound therapy, cognitive behavioral techniques, stress reduction, and hearing protection all play important roles in an effective treatment plan. Many patients find that while medications help manage specific aspects of tinnitus, these complementary approaches provide the foundation for long-term symptom control.
When evaluating tinnitus treatment claims, whether for prescription medications or supplements, maintain healthy skepticism. Look for evidence from well-designed clinical trials rather than anecdotal reports or marketing claims. The American Tinnitus Association and British Tinnitus Association maintain current, evidence-based information about treatment options and can help you separate promising approaches from those lacking scientific support.
Can any medication completely cure my tinnitus?
Currently, no medication has been proven to completely and permanently eliminate tinnitus for all patients. This reflects the complex, multifactorial nature of the condition rather than a lack of research effort. However, this doesn’t mean medications can’t help. In some cases—particularly when tinnitus stems from specific identifiable causes like inflammation, infection, or Meniere’s disease—appropriate medications may dramatically reduce or even resolve symptoms. For most chronic tinnitus cases, medications work best as part of a comprehensive management approach that includes addressing hearing loss, using sound therapy, and implementing psychological coping strategies rather than as standalone cures.
How long should I try a medication before deciding if it works?
The timeframe for evaluating medication effectiveness varies significantly depending on the type of medication and its mechanism of action. Antidepressants typically require 4-6 weeks to show their full benefit for tinnitus, while anti-anxiety medications may produce noticeable effects within days. Anti-inflammatory medications usually demonstrate their potential within 2-3 weeks. When starting any new tinnitus medication, establish clear expectations with your healthcare provider about the anticipated timeline for improvement and specific signs of effectiveness to monitor. Before concluding a medication isn’t helping, ensure you’ve taken it as prescribed for the full recommended trial period, as premature discontinuation might miss potential delayed benefits.
Are there any natural supplements proven to help tinnitus?
The evidence for natural supplements in tinnitus management remains limited and often contradictory. Melatonin shows the strongest scientific support, particularly for tinnitus patients with sleep disturbances. Zinc supplementation appears beneficial primarily for patients with documented zinc deficiency. Despite its popularity, ginkgo biloba has failed to demonstrate consistent benefits in well-designed clinical trials, though some patients with vascular risk factors report improvement. Magnesium supplementation shows theoretical promise based on its role in protecting against noise-induced hearing damage, but clinical evidence specifically for established tinnitus remains preliminary.
When considering supplements, quality matters tremendously. Choose products from reputable manufacturers that undergo independent testing for purity and potency. Always inform your healthcare providers about any supplements you’re taking, as some can interact with prescription medications or affect certain health conditions.
Can my regular doctor prescribe tinnitus medications or do I need a specialist?
Primary care physicians can prescribe many medications used for tinnitus management, particularly when the treatment approach is straightforward. However, for complex or severe cases, seeing a specialist often proves beneficial. Otolaryngologists (ENT doctors) can rule out medical conditions causing tinnitus and prescribe specialized treatments. Audiologists provide comprehensive tinnitus evaluations and sound-based therapies. Neurologists may offer additional insights for cases involving the central nervous system. The optimal approach often involves coordination between your primary doctor and appropriate specialists, ensuring both your tinnitus and overall health needs receive proper attention.
Will my insurance cover medications for tinnitus treatment?
- Prescription coverage typically depends on the medication prescribed rather than the condition being treated
- Medications prescribed for FDA-approved uses generally receive better coverage than off-label prescriptions
- Some insurers require prior authorization for certain tinnitus-related prescriptions
- Over-the-counter supplements are rarely covered by insurance
- Medicare Part D and most private insurance plans cover antidepressants and anti-anxiety medications when medically necessary
Insurance coverage for tinnitus treatments varies widely between plans and providers. When medication costs present a barrier, discuss this concern openly with your healthcare provider. Many medications used for tinnitus have generic alternatives that cost substantially less than brand-name versions. Additionally, patient assistance programs through pharmaceutical manufacturers or discount pharmacy cards can sometimes significantly reduce out-of-pocket expenses for necessary medications. For those exploring alternative treatments, consider reading about the effectiveness of Lipo-Flavonoid Plus for tinnitus relief.
If you encounter insurance denials for tinnitus medications, don’t hesitate to appeal. Request that your healthcare provider document how the medication addresses specific symptoms and improves functional status, as this detailed justification often helps overcome coverage limitations. For medications with established benefits for your particular situation, persistence often pays off in securing appropriate coverage. For more information on treatment options, you can refer to this WebMD article.
While medication offers important tools for managing tinnitus, the most successful approaches typically combine pharmacological treatments with other strategies like sound therapy, stress management, and cognitive techniques. Work closely with healthcare providers who understand these complementary approaches to develop a comprehensive plan tailored to your specific needs and symptoms.
For more comprehensive information about tinnitus management strategies beyond medication, Natural Remedies Guide offers personalized guidance on integrating pharmaceutical and non-pharmaceutical approaches for optimal symptom relief. Our commitment to evidence-based approaches ensures you receive the most current and effective treatment recommendations for your tinnitus journey.